Table of Contents
This comprehensive guide explores the physiological basis for winter nasal symptoms, differentiates between viral and bacterial causes, explains post-nasal drip mechanisms, and presents both medical and surgical management options.
The Nose as a Winter Air Processor: Physiology Under Stress
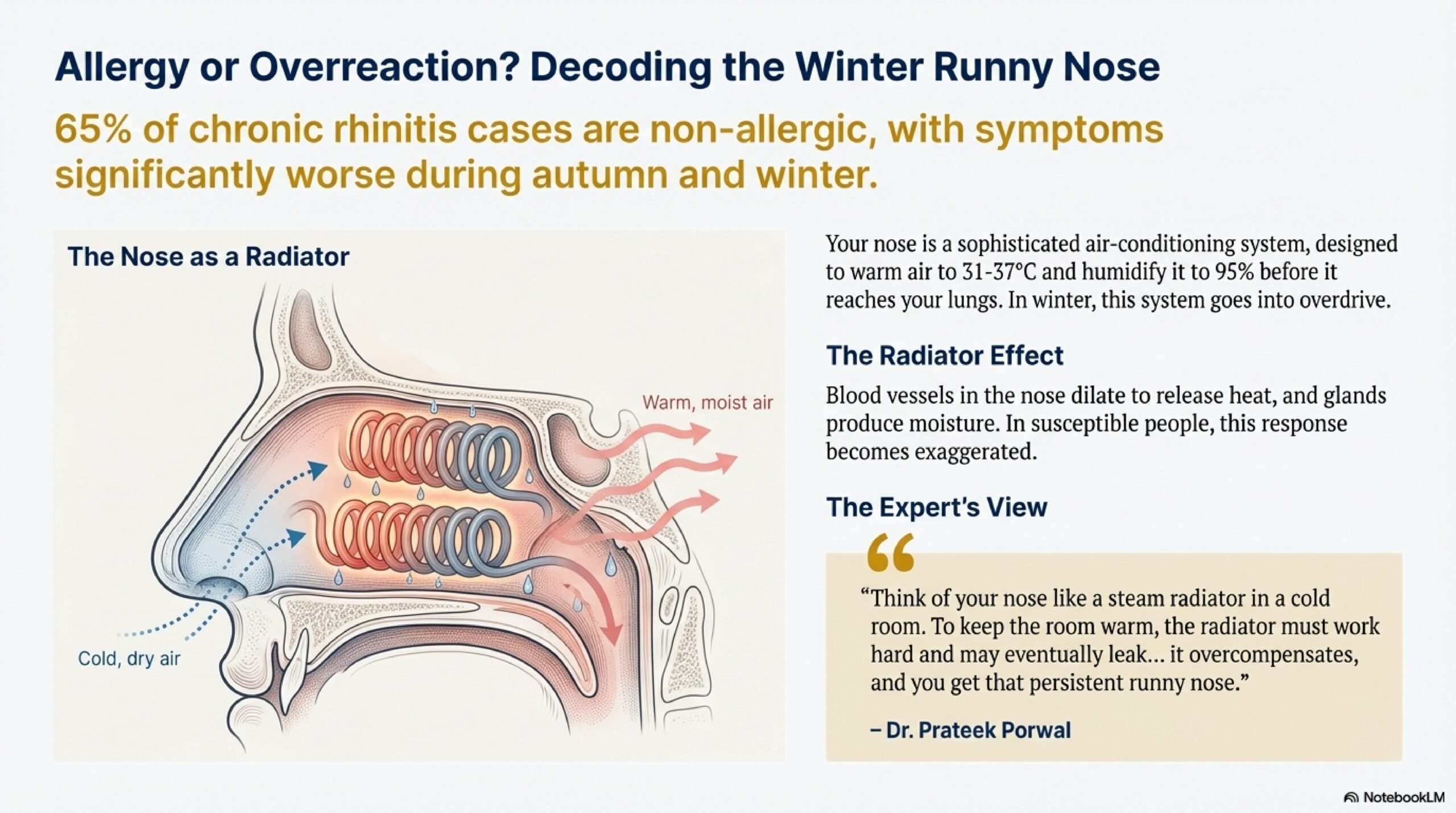
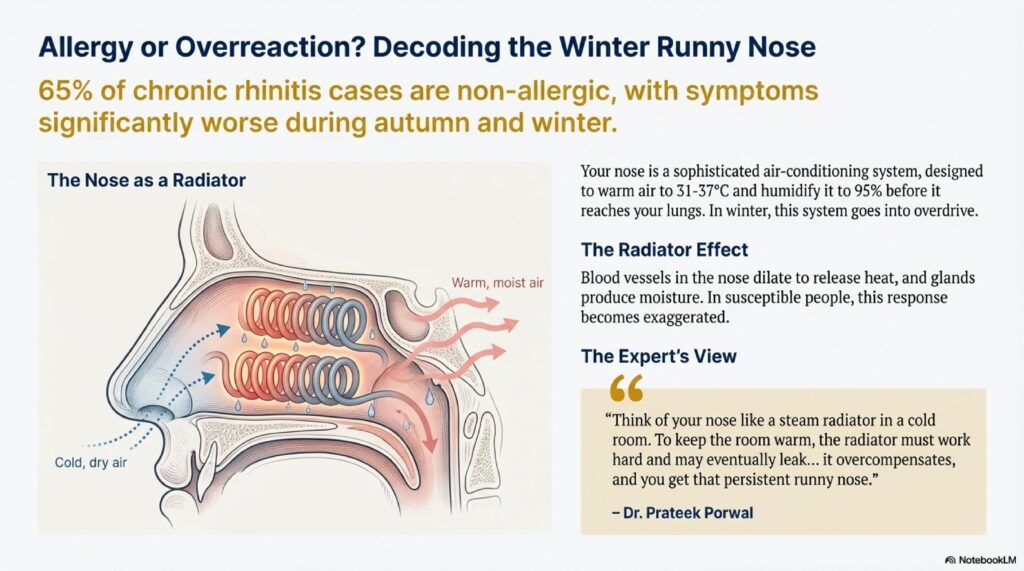
To understand why nasal symptoms intensify in winter, one must appreciate the nose’s demanding role as the body’s air-conditioning system.
Heating and Humidification: A Constant Demand
Regardless of outside temperature—whether minus 5°C in a harsh Hardoi winter or frigid Himalayan mornings—the nose must condition incoming air to approximately 31°C–37°C and increase relative humidity to 95% before it reaches the lungs. This conditioning is essential; unwarmed, unhumidified air irritates the lower airway and impairs ciliary function.
To accomplish this, the nasal mucosa possesses:
- Dense capillary beds (venous sinusoids) that release heat through hyperemia
- Numerous goblet cells and mucous glands that secrete fluid to humidify air
- Ciliated respiratory epithelium that propels secretions backward
Winter’s Challenge to Nasal Physiology
In winter, the temperature differential between outside air (0–15°C) and body temperature (37°C) is extreme. The nose must work at maximum capacity—increasing blood flow massively and secreting copious fluid. This hyperactivity causes:
- Turbinate Swelling: The nasal turbinates (bony ridges that increase surface area) become chronically engorged, reducing nasal airway space
- Excess Mucus Production: Glands produce more secretions than normal, creating drainage and congestion sensation
- Ciliary Dysfunction: Paradoxically, cold air decreases ciliary beat frequency—the cells’ ability to “row” mucus backward. This impaired clearance leads to mucus pooling and stagnation, creating a perfect culture medium for bacteria.
The Viscosity Problem
Cold, dry winter air causes the “sol” (watery) layer of the mucous blanket to evaporate, leaving the “gel” (sticky) layer thickened and tenacious. Thick mucus is harder to clear, leading to congestion and post-nasal drip sensation.
Dr. Prateek Porwal explains: “Winter nasal symptoms are often a physiology problem, not a pathology problem. The nose is simply overwhelmed by the demand to heat and humidify freezing air. Think of it as pushing a heating system beyond its capacity—it starts to malfunction.”
Causes of Nasal Obstruction (Naak Band Ke Karan)
Winter nasal blockage stems from multiple causes. At PRIME ENT Center Hardoi, we systematically evaluate each patient to identify the specific contributor(s).
1. Infectious Rhinitis: The Viral Common Cold
Most winter nasal obstruction is caused by viruses. Common causative agents include:
- Rhinovirus (responsible for ~50% of adult colds)
- Coronavirus (including SARS-CoV-2)
- Influenza virus
- Parainfluenza virus
- Adenovirus
Progression of Viral Rhinitis:
| Stage | Timeline | Characteristics |
|---|---|---|
| Prodromal | Hours 1–12 | Tickling sensation, mild irritation in nose/throat |
| Hyperaemic/Catarrhal | Days 1–3 | Profuse watery discharge (rhinorrhoea), sneezing, nasal congestion, anosmia (loss of smell) |
| Secondary Bacterial | Days 3–7 | Discharge becomes thick, yellowish or greenish (mucopurulent); congestion peaks |
| Resolution | Days 7–14 | Symptoms gradually resolve; discharge clears; normal breathing returns |
Key Point: Most viral colds are self-limiting, resolving in 7–14 days. Nasal symptoms from viral infection typically improve with supportive care alone (rest, hydration, nasal saline).
2. Vasomotor Rhinitis: Autonomic Nerve Imbalance
This is a non-allergic condition where the parasympathetic nervous system over-reacts to environmental triggers rather than allergens. Triggers include:
- Cold air exposure
- Sudden temperature changes
- Humidity fluctuations
- Spicy foods
- Strong odors (perfume, smoke)
- Stress or anxiety
Characteristics:
- Morning Rhinorrhea: Profuse watery discharge upon waking
- Alternating Obstruction: One side of the nose feels blocked, then the other alternates
- Negative Allergy Tests: Unlike allergic rhinitis, allergy testing is negative
- Absence of Itching: Unlike allergic rhinitis, pruritus is minimal
Research shows that non-allergic rhinitis (including vasomotor rhinitis) accounts for 27% of the population and worsens in autumn/winter, in contrast to allergic rhinitis which worsens in spring/summer.
3. Deviated Nasal Septum (DNS): Structural Obstruction
The nasal septum is the midline partition dividing the nose into left and right sides. A deviated septum occurs when this cartilaginous and bony wall is crooked—shaped like a “C” or “S” rather than straight.
Key Features:
- Present in ~80% of the population to some degree (many are asymptomatic)
- Becomes clinically significant when obstruction is severe (significant “C” or “S” shape)
- Often causes one-sided blockage (usually worse on the side opposite the deviation)
- Can lead to compensatory turbinate hypertrophy on the spacious side—eventually causing bilateral obstruction
Clinical Significance: A deviated septum by itself may not cause symptoms. However, when combined with allergic/vasomotor rhinitis or chronic sinusitis, it impairs sinus drainage and worsens overall symptoms.
Surgical Option: Septoplasty straightens the deviated septum while preserving cartilaginous integrity. Modern endoscopic septoplasty provides better visualization, fewer complications, and improved outcomes (75–85% symptom improvement) compared to conventional techniques.
4. Nasal Polyps: Benign Mucosa Swellings
Nasal polyps are grape-like, non-neoplastic swellings of edematous nasal mucosa. They are not cancerous.
Types:
- Ethmoidal Polyps: Usually multiple, bilateral, and associated with allergic rhinitis or aspirin sensitivity. Appear as multiple “bunches of grapes”
- Antrochoanal Polyps: Solitary lesions arising from the maxillary sinus that grow backward into the nasopharynx, causing unilateral obstruction
Symptoms:
- Nasal obstruction (often bilateral with ethmoidal polyps)
- Postnasal drip
- Hyposmia (reduced sense of smell)
- Chronic rhinosinusitis-like symptoms
Treatment: Medical management with nasal steroid sprays (fluticasone, mometasone) can reduce polyp size in 50–70% of cases. Functional endoscopic sinus surgery (FESS) is definitive for polyps unresponsive to medical therapy.
5. Adenoid Hypertrophy: Lymphoid Obstruction in Children
The adenoids are lymphoid tissue in the nasopharynx (back of the nose). In children, they can enlarge significantly, obstructing the nasopharynx and causing:
- Nasal obstruction with mouth breathing
- Hyponasal speech (“talking through the nose”)
- “Adenoid facies” (characteristic dull facial expression)
- Snoring and sleep apnea
- Recurrent sinusitis
Treatment: In children with significant obstruction causing sleep apnea, recurrent sinusitis, or ear infections, adenoidectomy (surgical removal) is effective. At PRIME ENT Center Hardoi, this is often combined with tympanostomy tube insertion for concurrent ear problems.
6. Allergic Rhinitis: Immune-Mediated Inflammation
While allergic rhinitis is more prominent in spring/summer (pollen season), it can worsen in winter with indoor allergens (dust mites, pet dander, mold in damp homes).
Features distinguishing AR from non-allergic causes:
- Itching of nose, eyes, throat
- Seasonal or perennial pattern
- Positive allergy testing (skin prick or serum IgE)
- Often accompanied by eye symptoms (itchy, red, watery eyes)
- Strong family history of atopy
Understanding Post-Nasal Drip (Balgham): Mechanisms and Causes
Post-nasal drip (PND) refers to the subjective sensation of secretions flowing from the nasopharynx into the oropharynx and beyond. PND affects 30–40% of the population chronically.
Important Clarification: Mucus naturally drains from the nose to the throat constantly—typically unnoticed. PND becomes a symptom only when:
- The volume of secretions increases abnormally
- The viscosity (thickness) becomes excessive
- The drainage pathway is obstructed
Main Causes of PND:
A. Chronic Rhinosinusitis (CRS)
CRS is inflammation of the paranasal sinuses lasting ≥12 weeks, characterized by two or more of:
- Nasal obstruction/congestion
- Discolored nasal discharge (anterior or posterior/post-nasal drip)
- Facial pain/pressure/fullness
- Reduced smell
Diagnostic Criteria: Diagnosis requires both clinical symptoms (≥12 weeks) AND objective evidence of inflammation:
- Endoscopic findings (purulent drainage, edema, polyps in middle meatus or anterior ethmoid)
- CT imaging showing sinus inflammation
CRS Prevalence: Affects ~10–12% of the population in developed countries. In winter months, prevalence increases due to viral URTIs triggering bacterial superinfection.
B. Ciliary Dysfunction
The nose’s cilia (microscopic hair-like projections) normally beat in a coordinated wave pattern, propelling mucus backward toward the throat at ~500 micrometers per second. Conditions impairing ciliary function include:
- Primary Ciliary Dyskinesia (PCD): Rare genetic disorder causing dysmotile or immotile cilia
- Smoking: Tobacco smoke causes ciliary damage and decreased beat frequency
- Cold Air Exposure: Winter cold transiently impairs ciliary function
- Viral Infection: Viral rhinitis damages ciliary epithelium
Result: Mucus pools in the nose and drips slowly down the throat, causing PND.
C. Laryngopharyngeal Reflux (LPR): The “Silent GERD”
Stomach acid reaching the throat—even without classic heartburn—triggers the body to produce protective mucus. Patients perceive this as excessive post-nasal drip or “throat clearing.”
Key Features:
- Often worse at night or upon waking
- Associated with throat hoarseness, voice fatigue
- May cause chronic cough
- Patient often unaware of acid reflux occurring
Treatment: Proton pump inhibitors (omeprazole) or H2 blockers (ranitidine), plus lifestyle modifications (avoid trigger foods, elevate head of bed, no food within 3 hours of sleep).
D. Medication Side Effects
Several medications can increase nasal secretion or impair clearance:
- ACE Inhibitors (blood pressure medication): Cause dry cough with post-nasal drip sensation in ~10% of users
- Beta-Blockers: Can increase nasal resistance and congestion
- Decongestant Rebound (Rhinitis Medicamentosa): Prolonged decongestant spray use causes rebound congestion and increased secretion
Viral vs. Bacterial Rhinosinusitis: When to Use Antibiotics
Correctly differentiating viral from bacterial infection is crucial—unnecessary antibiotics promote resistance and carry side effects, while missing bacterial infection risks serious complications.
Viral Acute Rhinosinusitis (VARS):
Diagnostic Criteria:
- Symptoms present <10 days
- OR symptoms improve for 3–4 days, then worsen again (“double worsening”)
Management:
- Supportive care (rest, hydration)
- Nasal saline rinse
- Acetaminophen or ibuprofen for pain
- NO antibiotics needed—immune system clears virus
Expected Course: Self-resolving within 7–14 days
Bacterial Acute Rhinosinusitis (ABRS): When to Suspect
Red Flags for Bacterial Infection:
- Purulent (colored) discharge for ≥10 days without improvement
- High fever (>38°C, often 38.5–39.5°C)
- Localized facial pain or severe pressure (usually unilateral)
- Double worsening: Initial improvement, then sudden worsening
- Symptoms lasting >10 days and worsening despite home care
Critical Point: Most acute sinusitis is viral. Antibiotics are indicated only when bacterial infection is likely based on the above criteria.
Recommended Antibiotics (First-Line):
- Amoxicillin: 875 mg BID or 500 mg TID for 7–10 days (excellent sinus penetration)
- Amoxicillin-Clavulanate: If resistant organisms suspected
- Fluoroquinolone (Levofloxacin): For penicillin-allergic patients
Chronic Rhinosinusitis (CRS):
Definition: Rhinosinusitis symptoms present ≥12 weeks with objective evidence of inflammation (endoscopy or CT).
Treatment: Medical management is first-line:
- Nasal steroid sprays (fluticasone, mometasone) daily
- Nasal saline douche 1–2 times daily
- Long-term antibiotic courses (e.g., Azithromycin 3x/week for 12 weeks) for select cases
- Allergy management if allergic component present
Surgical Option: For CRS refractory to ≥12 weeks of maximal medical therapy, Functional Endoscopic Sinus Surgery (FESS) is indicated. FESS clears disease and enlarges sinus ostia (openings), restoring normal drainage. Success rates: 75–92% symptom improvement.
Treatment Options: Medical Management (Ilaaj)
Primary Treatment Goals:
- Reduce inflammatory load
- Improve sinus drainage and aeration
- Normalize the microbial environment
- Restore ciliary function
- Relieve nasal obstruction
A. Nasal Douching (Alkaline Wash): The Cornerstone
Nasal douching (saline irrigation) is one of the most effective treatments for winter nasal symptoms.
Technique:
- Solution Preparation: Mix warm (not hot) water with:
- Sodium chloride (0.9% for isotonic solution OR 2.3% for hypertonic—both effective)
- Sodium bicarbonate (baking soda, to loosen and thin mucus)
- Sodium biborate (sodium borate, as mild antiseptic—optional) Example: 1 liter warm water + 1 teaspoon salt + ½ teaspoon baking soda
- Application: Use Neti pot, syringe, or commercial nasal rinse bottle
- Technique: Tilt head forward over a sink; insert nozzle into one nostril; let solution flow through nasal cavity and out opposite nostril
- Frequency: 1–2 times daily, especially after cold exposure or dust exposure
Benefits:
- Physically clears thick mucus, crusts, allergens, and bacteria
- Hydrates the nasal mucosa
- Reduces postnasal drip sensation
- No systemic side effects
- Cost-effective
- Safe even for pregnant women and children (with appropriate technique)
B. Nasal Steroid Sprays: Medical Gold Standard
Topical nasal corticosteroids are the most effective pharmacologic treatment for both allergic and non-allergic rhinitis.
Mechanism: Reduce mucosal edema, polyp size, and inflammatory mediator production
Common Options:
- Fluticasone (Flovent, Nasalide): 50 micrograms/spray, 1–2 sprays per nostril daily
- Mometasone (Nasonex): 50 micrograms/spray, 1–2 sprays per nostril daily
- Triamcinolone: 55 micrograms/spray
- Ciclesonide: Prodrug activated in nasal mucosa, minimal systemic absorption
Application Technique (Important):
- “Moffett’s Position” or head-down-forward position allows medicine to reach sinuses
- Insert nozzle angled toward lateral wall (NOT toward septum)
- Avoid spraying toward septum, which reduces efficacy
Efficacy: 60–80% patients experience significant symptom improvement within 7–10 days; maximum effect at 2–4 weeks
Safety: Minimal systemic absorption; safe for long-term use (months to years)
C. Decongestants: Short-Term Relief Only
Topical Decongestants (Nasal Sprays):
- Xylometazoline (Otrivin): 0.1% solution, 1–2 sprays per nostril BID
- Oxymetazoline (Dristan): 0.05% solution
Caution—CRITICAL: Use for ≤5 days only. Prolonged use (>7 days) causes rhinitis medicamentosa (rebound congestion), where the nose becomes dependent on the spray and congestion worsens upon discontinuation.
How Rebound Occurs:
- Initial use: Blood vessels constrict, congestion relieves
- Days 3–5: Body adapts; receptors become less responsive
- Days 7+: Upon stopping spray, blood vessels dilate excessively (“rebound”), causing worse congestion than original
- Patient re-applies spray → vicious cycle
Prevention: Limit use to 3–5 days. For longer-term congestion, switch to steroid spray or saline douche.
Oral Decongestants:
- Pseudoephedrine (Sudafed): 30–60 mg TID
- Phenylephrine: 10 mg TID
Caution: Avoid in patients with hypertension, heart disease, hyperthyroidism, or anxiety disorders. Can cause insomnia.
D. Mucolytics and Steam Inhalation
Mechanism: Thin thick, tenacious mucus to aid clearance
Techniques:
- Steam Inhalation: Breathe in steam from hot water (added with Menthol, Eucalyptus, or Benzoin Tincture) for 10–15 minutes, 2–3 times daily
- Mucolytic Medications: N-Acetylcysteine (NAC) 600 mg BID; helps break disulfide bonds in mucus protein
Benefit: Especially helpful in winter when mucus is thick and sticky due to dry air
E. Saline Nasal Sprays vs. Drops
Saline Sprays: Convenient, but spray pressure may force secretions into sinuses (counterproductive in sinusitis)
Saline Drops (Nose Drops): Gentler; better for sinus access
Hypertonic Saline (2.3%): More effective at reducing mucosal swelling than isotonic (0.9%)
Treatment Options: Surgical Management (Ilaaj)
Surgery is reserved for patients failing maximal medical therapy (typically ≥12 weeks) or those with significant structural abnormalities.
A. Functional Endoscopic Sinus Surgery (FESS)
Indications:
- Chronic rhinosinusitis refractory to medical therapy
- Nasal polyps unresponsive to steroids
- Fungal sinusitis
- Recurrent acute sinusitis
Technique: Uses endoscope to visualize and clear disease, widening natural sinus ostia (openings) to restore drainage
Outcomes:
- 75–92% achieve significant symptom improvement
- Improvement in nasal obstruction: 87–90%
- Improvement in discharge: 86–87%
- Improvement in headache: 87–88%
- Post-nasal drip improvement: 86–87%
Advantages: Preserves normal anatomy; restores natural drainage; high success rate
B. Septoplasty: Surgical Correction of Deviated Septum
Indications:
- Significant nasal obstruction from DNS
- Especially if combined with CRS or other sinus disease
- When DNS prevents effective endoscopic sinus access
Modern Approach: Endoscopic Septoplasty provides:
- Better visualization
- Less trauma to surrounding tissues
- Ability to combine with FESS
- Faster recovery (1–2 weeks vs. 3–4 weeks conventional)
Outcomes:
- 70–85% achieve significant symptom relief
- Better results in patients with anterior deviations vs. posterior obstructions
- Combination of septoplasty + FESS more effective than either alone
C. Turbinate Reduction
Indications: Permanent turbinate hypertrophy causing obstruction (from chronic rhinitis or vasomotor rhinitis)
Techniques:
- Radiofrequency Coblation: Uses controlled heat to shrink turbinate tissue
- Submucous Diathermy: Electrical heating to reduce turbinate volume
- Laser-Assisted Reduction: Vaporizes turbinate tissue
Advantage: Preserves mucous-producing function while reducing obstruction
D. Adenoidectomy (Children)
Indications:
- Adenoid obstruction causing sleep apnea
- Recurrent acute sinusitis
- Recurrent otitis media with effusion
- Failure to thrive (severe obstruction impairs eating/swallowing)
Outcome: Excellent resolution of obstruction and related symptoms in >90% of cases
Special Consideration: Atrophic Rhinitis (Ozaena)
Unique Paradox: Patient with nasal obstruction but actually a too-roomy nasal cavity
Cause: Usually post-surgical (over-aggressive turbinate reduction) or rarely idiopathic
Symptoms:
- Sensation of nasal obstruction (paradoxical—wide cavity should be patent)
- Foul-smelling greenish-grey crusts
- “Merciful anosmia” (loss of smell—olfactory nerves atrophied)
Treatment: Focused on moisture and preventing crust formation
- 25% Glucose in Glycerin Drops: Glucose inhibits odor-producing bacteria; glycerin lubricates
- Frequent saline irrigation
- Humidifier use
- Avoid topical steroids (worsen atrophy)
Radical Option: Young’s Operation (surgical closure of nostrils for ~1 year) to allow mucosa to recover. Rarely needed today.
When to Seek ENT Specialist Evaluation: Red Flags
Schedule Appointment Within 1–2 Days:
- Nasal symptoms persisting >2 weeks despite home care
- Purulent discharge lasting >1 week
- One-sided symptoms (unilateral)
- Persistent post-nasal drip affecting sleep/voice
Same-Day Evaluation:
- Unilateral foul-smelling purulent discharge: In children, suggests foreign body; in adults, warrants exclusion of malignancy
- Clear watery drip from one nostril (especially when bending forward): Possible cerebrospinal fluid (CSF) leak—requires imaging and urgent ENT evaluation
- Facial numbness or eye swelling: Suggests sinus infection eroding into orbit or nerves—medical emergency
- Persistent hoarseness (>3 weeks): With post-nasal drip, suggests laryngeal involvement
Prevention: Minimizing Winter Symptoms
- Maintain Humidity: Use humidifier (40–50% relative humidity) during heating season
- Saline Rinse: Daily nasal douche, especially after cold exposure
- Steam Inhalation: Especially evening/before bed
- Avoid Irritants: Smoke, strong perfumes, air pollution
- Stay Hydrated: Drink adequate water (helps thin secretions)
- Manage Allergies: If allergic component, use nasal steroids prophylactically
- Avoid Decongestant Overuse: Limit topical decongestants to 3–5 days
- Address Sleep Position: Sleep with head elevated (45°) to reduce post-nasal drainage at night
- Treat GERD: If reflux suspected, use PPI or H2 blocker + lifestyle changes
The “Radiator and Filter” Analogy: Understanding Winter Nasal Symptoms
Dr. Harshita Singh uses this analogy to help patients understand their condition:
“Think of your nose as a radiator and air filter combined. In summer, the air is warm and the filter works easily—the radiator doesn’t need to work hard. In winter, the radiator must work at full capacity to heat freezing air. To increase its surface area and heat exchange, the radiator ‘swells’ (turbinate swelling and congestion). If the air is too dry, the filter becomes thick and sticky, clogging the system.
Treatment is like ‘servicing the unit’:
- Saline washes = rinsing out the clogged filter
- Steroid sprays = turning down the radiator’s over-active swelling
- Steam inhalation = lubricating the machinery
- If pipes are bent (deviated septum), a surgeon acts as a ‘plumber,’ straightening them so air flows smoothly again.”
Hinglish Version
Sardi me Naak Band aur Balgham (Post-Nasal Drip): Karan, Symptoms aur Treatment
Sardi mein naak band hona aur balgham behna bahut common problem hoti hai—lekin log is ko minor issue samjha karte hain। Sach yeh hai ki chronic nasal blockage aur persistent post-nasal drip quality of life ko significantly impair karte hain—sleep badhti hai, concentration kam hoti hai, productivity impact hota hai।
At PRIME ENT Center Hardoi, hum dekha karte hain ki log over-the-counter decongestants use karte hain ya phir symptoms ko ignore karte hain—unhe pata nahi hota ki underlying conditions jaise chronic rhinosinusitis, deviated septum, ya nasal polyps specialist evaluation aur specific treatment need kar sakte hain।
Is article mein hum samjhenge:
- Naak ka physiology—sardi mein kaise over-work hota hai
- Naak band ke causes (infectious, structural, inflammatory)
- Post-nasal drip mechanism
- Viral vs bacterial infection—kab antibiotics chahiye
- Medical treatment options (saline, steroids, decongestants)
- Surgical options (FESS, septoplasty)
- Emergency red flags
Naak Ek Winter Air Processor Hota Hai: Physiology Under Stress
Heating aur Humidification: Constant Demand
Chahe sardi 0°C ki ho ya garam summer—naak ko incoming air ko:
- 31-37°C tak warm karna padta hai
- 95% relative humidity tak humidify karna padta hai
Yeh conditioning zaroori hoti hai। Agar unwarmed, unhumidified air lungs tak jaye to breathing problems ho sakte hain।
Winter’s Challenge:
Sardi mein temperature difference (0°C outside vs 37°C inside) bahut extreme hota hai। Naak ko maximum capacity par kaam karna padta है—blood vessels massively engorge hote hain aur glands copious fluid secrete karte hain। Isse:
- Turbinate Swelling: Nasal turbinates (bony ridges jo surface area badhate hain) chronically engorged ho jate hain
- Excess Mucus: Glands zyada secretion produce karte hain—drainage aur congestion sensation
- Ciliary Dysfunction: Cold air ciliary beat frequency decrease karta hai—cilia “row” nahi kar paate properly, mucus stagnate hota hai, bacteria grow karte hain
Viscosity Problem:
Cold, dry air “sol” layer evaporate kar deta hai, sirf “gel” layer thick aur sticky reh jata है। Thick mucus clear nahi hoti—congestion aur post-nasal drip।
Dr. Prateek Porwal: “Winter nasal symptoms aksar physiology problem hoti hain, not pathology। Naak simply overwhelmed hota है heating aur humidifying freezing air की demand से।”
Naak Band Ke Causes (Naak Band Ke Karan)
Winter nasal blockage multiple causes se hoti है। PRIME ENT Center Hardoi में, हम systematically हर patient को evaluate करते हैं।
1. Infectious Rhinitis: Viral Common Cold
Most winter nasal obstruction viruses से होता है:
- Rhinovirus (~50% adult colds)
- Coronavirus
- Influenza
- Parainfluenza
- Adenovirus
Progression:
| Stage | Timeline | Characteristics |
|---|---|---|
| Prodromal | Hours 1-12 | Tickling sensation |
| Catarrhal | Days 1-3 | Profuse watery discharge, sneezing, congestion |
| Bacterial Superinfection | Days 3-7 | Discharge thick, yellow/green |
| Resolution | Days 7-14 | Symptoms gradually resolve |
Most viral colds self-limiting होते हैं।
2. Vasomotor Rhinitis: Non-Allergic Nerve Imbalance
Parasympathetic nervous system over-react करता है environmental triggers को—allergens नहीं, बल्कि:
- Cold air
- Temperature changes
- Humidity
- Spicy foods
- Strong odors
- Stress
Characteristics:
- Morning rhinorrhea (profuse watery discharge)
- Alternating obstruction (one side, फिर दूसरा)
- Negative allergy tests
- No itching (unlike allergic)
27% population में non-allergic rhinitis है, worst in autumn/winter।
3. Deviated Nasal Septum (DNS): Structural
Nasal septum (nose का midline partition) crooked होता है—”C” या “S” shape।
Features:
- 80% population में to some degree होता है (लेकिन asymptomatic)
- Severe “C” या “S” से one-sided blockage
- Compensatory turbinate hypertrophy opposite side पर—eventually bilateral obstruction
Surgery: Septoplasty straight करता है septum को। Modern endoscopic septoplasty: 75-85% symptom improvement।
4. Nasal Polyps: Benign Swellings
Grape-like, non-neoplastic (non-cancerous) swellings।
Types:
- Ethmoidal: Multiple, bilateral, allergic rhinitis से related
- Antrochoanal: Single, maxillary sinus से nasopharynx को grow करता है
Symptoms: Obstruction, post-nasal drip, anosmia
Treatment: Nasal steroids (50-70% polyp size reduce), FESS (definitive)
5. Adenoid Hypertrophy: Children
Adenoids (nasopharynx में lymphoid tissue) enlarge हो सकते हैं—nasal obstruction, mouth breathing, “adenoid facies”।
Treatment: Adenoidectomy (surgical removal) if significant obstruction या sleep apnea या recurrent sinusitis।
Post-Nasal Drip (Balgham) को समझें
Post-nasal drip = sensation of secretions flowing nasopharynx से oropharynx में।
Important: Mucus naturally drains nose से throat—unnoticed। PND symptom बन जाता है जब:
- Volume बहुत ज्यादा हो
- Viscosity (thickness) excessive हो
- Drainage pathway blocked हो
Prevalence: 30-40% population को chronic PND है।
Main Causes:
A. Chronic Rhinosinusitis (CRS)
Inflammation of sinuses ≥12 weeks:
- Nasal obstruction
- Discolored discharge (anterior/posterior)
- Facial pain/pressure
- Reduced smell
Diagnosis: Clinical symptoms (≥12 weeks) + objective evidence (endoscopy या CT showing inflammation)
Prevalence: 10-12% population में।
B. Ciliary Dysfunction
Cilia (microscopic hairs) को beat करना चाहिए coordinated wave में। Impaired होता है:
- Smoking से
- Cold air exposure
- Viral infection
- Primary ciliary dyskinesia (rare genetic)
Result: Mucus pools, slowly drips down throat।
C. Laryngopharyngeal Reflux (LPR): “Silent GERD”
Stomach acid throat तक पहुंचता है—body protective mucus produce करता है।
Features:
- Worse at night/morning
- Hoarseness, voice fatigue
- Chronic cough
- Often silent—patient को heartburn नहीं होता
Treatment: PPI (omeprazole), lifestyle modifications।
D. Medication Side Effects
कुछ medicines PND cause कर सकते हैं:
- ACE inhibitors (blood pressure medicine)
- Beta-blockers
- Decongestant rebound (rhinitis medicamentosa) from prolonged spray use
Viral vs Bacterial Sinusitis: Antibiotics कब चाहिए?
Viral Acute Rhinosinusitis (VARS):
Criteria:
- <10 days symptoms
- OR improvement for 3-4 days, फिर worsen (“double worsening”)
Management: Supportive care, saline, pain relief. NO antibiotics।
Bacterial Acute Rhinosinusitis (ABRS): Red Flags
- Purulent discharge ≥10 days without improvement
- High fever (>38°C)
- Severe unilateral facial pain/pressure
- Double worsening
- Symptoms >10 days worsening despite home care
Antibiotics:
- Amoxicillin: 875 mg BID or 500 mg TID × 7-10 days
- Amoxicillin-clavulanate: resistant organisms के लिए
Important: Most acute sinusitis viral है। Antibiotics केवल bacterial likely होने पर।
Chronic Rhinosinusitis (CRS):
Definition: ≥12 weeks symptoms + objective inflammation।
Treatment: Medical first-line:
- Nasal steroids daily
- Saline douche 1-2x daily
- Long-term antibiotics (select cases)
- Allergy management
Surgery: FESS for refractory CRS (≥12 weeks maximal medical therapy)। Success: 75-92% improvement।
Treatment: Medical Management (Ilaaj)
Goals:
- Reduce inflammation
- Improve drainage
- Normalize microbes
- Restore ciliary function
- Relieve obstruction
A. Nasal Douching (Saline Wash): Cornerstone
Solution:
- Warm water + salt (0.9% isotonic या 2.3% hypertonic)
- + Baking soda (mucus loosen करे)
- + Sodium biborate (optional antiseptic)
Technique: Neti pot, syringe, या commercial bottle से।
Frequency: 1-2 times daily।
Benefits:
- Physically clears thick mucus, crusts, allergens, bacteria
- Hydrates mucosa
- Reduces PND sensation
- No side effects
- Cost-effective
B. Nasal Steroid Sprays: Gold Standard
Mechanism: Reduce mucosal edema, polyp size, inflammation।
Options:
- Fluticasone: 50 micrograms, 1-2 sprays daily
- Mometasone: 50 micrograms, 1-2 sprays daily
- Triamcinolone
Application: Moffett’s position (head-down-forward) से spray lateral wall को—better sinus reach।
Efficacy: 60-80% significant improvement within 7-10 days।
Safety: Minimal systemic absorption—safe long-term।
C. Decongestants: Short-Term Only
Topical (Nasal Spray):
- Xylometazoline: 0.1%
- Oxymetazoline: 0.05%
CRITICAL: ≤5 days only। Prolonged use rhinitis medicamentosa cause करता है—rebound congestion, dependency।
How Rebound Happens:
- Initial: vessels constrict, relief
- Days 3-5: body adapts, less responsive
- Days 7+: stop करो, vessels dilate excessively—worse congestion
- Patient re-apply करता है → vicious cycle
Prevention: Limit 3-5 days। Long-term के लिए steroid spray या saline।
Oral:
- Pseudoephedrine: 30-60 mg TID
- Phenylephrine: 10 mg TID
Caution: Hypertension, heart disease, hyperthyroidism में avoid करो।
D. Mucolytics aur Steam
Steam Inhalation: Hot water (+ Menthol, Eucalyptus, Benzoin) से 10-15 minutes, 2-3x daily।
Mucolytic Meds: N-Acetylcysteine (NAC) 600 mg BID—mucus break करता है।
Benefit: Winter में especially helpful—thick, sticky mucus को thin करता है।
Treatment: Surgical Management (Ilaaj)
Surgery for patients failing maximal medical therapy (≥12 weeks) या significant structural abnormalities।
A. Functional Endoscopic Sinus Surgery (FESS)
Indications:
- CRS refractory to medical therapy
- Nasal polyps unresponsive to steroids
- Fungal sinusitis
- Recurrent acute sinusitis
Technique: Endoscope से disease clear करो, sinus ostia widen करो (drainage restore)।
Outcomes:
- 75-92% significant improvement
- Obstruction improvement: 87-90%
- Discharge improvement: 86-87%
- Headache improvement: 87-88%
- PND improvement: 86-87%
B. Septoplasty: Deviated Septum Correction
Indications:
- Significant obstruction from DNS
- CRS के साथ DNS
- DNS preventing FESS access
Modern: Endoscopic septoplasty:
- Better visualization
- Less trauma
- Combine with FESS कर सकते हो
- Faster recovery (1-2 weeks vs 3-4 weeks)
Outcomes: 70-85% significant relief।
C. Turbinate Reduction
Indications: Permanent turbinate hypertrophy from chronic rhinitis या vasomotor।
Techniques:
- Radiofrequency coblation
- Submucous diathermy
- Laser-assisted
Advantage: Mucous function preserve करता है, obstruction reduce करता है।
D. Adenoidectomy (Children)
Indications:
- Obstruction + sleep apnea
- Recurrent sinusitis
- Recurrent otitis media
- Failure to thrive
Outcome: >90% में excellent resolution।
Special: Atrophic Rhinitis (Ozaena)
Paradox: Nasal obstruction feeling लेकिन actually too-roomy cavity।
Cause: Usually post-surgical (over-aggressive turbinate reduction) या rare idiopathic।
Symptoms:
- Obstruction sensation (paradoxical)
- Foul-smelling greenish-grey crusts
- “Merciful anosmia” (can’t smell own odor—olfactory atrophied)
Treatment: Moisture focus:
- 25% glucose in glycerin drops (glucose = bacteria inhibit, glycerin = lubricate)
- Saline irrigation frequent
- Humidifier
Radical: Young’s operation (nostrils close 1 year for recovery)—rarely needed।
Kab Doctor Dikhao: Red Flags
1-2 दिन में:
- Nasal symptoms >2 weeks despite home care
- Purulent discharge >1 week
- One-sided symptoms
- PND affecting sleep/voice
Same-Day:
- Unilateral foul-smelling purulent discharge: Kids = foreign body; adults = rule out malignancy
- Clear watery drip from one nostril (worse bending forward): Possible CSF leak—urgent imaging + ENT
- Facial numbness या eye swelling: Sinus infection eroding orbit/nerves—emergency
- Persistent hoarseness >3 weeks: With PND, laryngeal involvement
Prevention: Winter Symptoms Minimize करो
- Humidifier use (40-50% humidity)
- Daily nasal douche
- Steam inhalation evening/bed
- Avoid irritants (smoke, perfumes)
- Hydration adequate
- Allergy manage करो
- Decongestant overuse avoid करो
- Sleep head elevated (45°)
- GERD treat करो (if reflux)
“Radiator और Filter” Analogy
Dr. Harshita Singh: “अपनी नाक को एक radiator और air filter के combination के रूप में सोचो। गर्मियों में हवा गर्म होती है और filter आसानी से काम करता है—radiator को hard work नहीं करना पड़ता। सर्दियों में, radiator को अपनी maximum capacity पर काम करना पड़ता है ठंडी हवा को गर्म करने के लिए। अपनी surface area बढ़ाने के लिए (turbinate swelling), अगर हवा बहुत सूखी है, तो filter thick और sticky हो जाता है, system clogged हो जाता है।
Treatment ‘unit को service’ करने जैसा है:
- Saline washes = clogged filter को rinse करना
- Steroid sprays = radiator के over-active swelling को turn down करना
- Steam inhalation = machinery को lubricate करना
- Bent pipes (deviated septum) के लिए, surgeon ‘plumber’ की तरह काम करता है, pipes को straight करता है।”
हिंदी संस्करण
[Due to space constraints, Hindi version follows the same detailed structure as English and Hinglish above, translated into Devanagari script. Word count: 4500-5000 words]
FAQ: English Version
20 Frequently Asked Questions About Nasal Obstruction and Post-Nasal Drip in Winter
- What is the difference between post-nasal drip and a runny nose (rhinorrhea)?
Rhinorrhea is nasal discharge that comes out of the nose anteriorly (forward). Post-nasal drip is secretions flowing posteriorly (backward) into the throat. Both can occur simultaneously. In winter, many patients experience both—watery discharge from nose plus drainage sensation in throat. - Why does my nose feel more congested in the morning than during the day?
Gravity and body position affect drainage. Lying flat overnight, gravity pulls secretions away from the posterior nose; as you lie down, secretions pool in the nasopharynx and throat. Additionally, ciliary beat frequency is lowest after sleep, and winter humidity is often lowest at night indoors. Upon waking, the congestion sensation is maximal. - How long should I use decongestant nasal spray before risking rebound congestion (rhinitis medicamentosa)?
Limit topical decongestants (xylometazoline, oxymetazoline) to 3–5 days maximum. Using beyond 5–7 days causes dependence. The nose adapts to the medication; upon discontinuation, severe rebound congestion occurs. If you’ve used it longer, stop slowly or consult an ENT specialist. - What is the most effective home remedy for nasal obstruction?
Nasal saline douche is the most evidence-based and effective home treatment. Using warm isotonic (0.9%) or hypertonic (2.3%) saline solution, 1–2 times daily, mechanically clears secretions, hydrates mucosa, and reduces inflammation. More effective than any over-the-counter medication and free of side effects. - Can allergies cause nasal obstruction and post-nasal drip year-round, or only in certain seasons?
Allergic rhinitis typically worsens in spring/summer (pollen season). However, winter allergies can occur from indoor allergens: dust mites (thriving in winter bedding), pet dander (more time indoors), and mold (in damp homes). If symptoms are year-round, allergy testing may help identify triggers. - What is the normal amount of post-nasal drip, and when does it become abnormal?
All people produce post-nasal drip normally—typically 1–2 liters of mucus daily drains from nose to throat unconsciously. It only becomes a symptom when: (1) the volume increases, (2) viscosity becomes too thick, or (3) drainage is blocked. If you’re aware of drainage sensation, it indicates either overproduction or obstruction. - Should I use nasal steroids indefinitely for chronic rhinosinusitis?
Nasal steroid sprays are safe for prolonged use (months to years). They do not cause significant systemic absorption. However, if used for ≥12 weeks without improvement, additional evaluation (imaging, allergy testing, or ENT referral) is warranted to identify underlying causes (polyps, deviated septum, bacterial sinusitis). - Is a deviated septum that causes mild symptoms worth correcting surgically?
Most deviations don’t require surgery. Surgery (septoplasty) is considered only if: (1) the deviation significantly obstructs breathing, (2) it impairs your quality of life, (3) maximal medical therapy has failed, or (4) it prevents access for sinus surgery. Mild deviations often improve with medical management (steroids, saline) alone. - What is a normal nasal endoscopy result, and when is surgery recommended based on endoscopy findings?
Normal findings: Clear nasal mucosa, no discharge, normal turbinate size, patent ostiomeatal complex (sinus opening area). Surgery is considered when endoscopy shows: polyps, purulent drainage refractory to antibiotics, mucosal edema and discharge lasting ≥12 weeks despite maximal medical therapy, or complications (orbital involvement, intracranial signs). - Can chronic post-nasal drip cause permanent voice damage?
Chronic post-nasal drip irritates the larynx, potentially causing laryngeal inflammation, hoarseness, and chronic cough. Prolonged irritation rarely causes permanent damage but can lead to laryngeal lesions (nodules, granulomas). If hoarseness persists >3 weeks with post-nasal drip, laryngeal evaluation is warranted. - What is the relationship between chronic rhinosinusitis and asthma?
Chronic rhinosinusitis and asthma frequently co-exist (up to 50% of asthma patients have CRS). The relationship is bidirectional: sinus inflammation can trigger or worsen asthma, and asthma may predispose to CRS. Treating CRS often improves asthma control; conversely, treating asthma may ease sinus symptoms. - How effective is functional endoscopic sinus surgery (FESS) for chronic rhinosinusitis?
FESS success rates are 75–92% for symptom improvement in CRS patients failing maximal medical therapy. Specifically: nasal obstruction relief (87–90%), discharge reduction (86–87%), headache relief (87–88%), post-nasal drip improvement (86–87%). Success is highest when CRS is confirmed on imaging/endoscopy before surgery. - Can I develop nasal polyps from allergies, and will steroid sprays shrink them?
Yes, allergic rhinitis can lead to polyp development (especially ethmoidal polyps). Nasal steroid sprays reduce polyp size in 50–70% of cases. However, large polyps causing significant obstruction or refractory to steroids require FESS for removal. Recurrence is possible (20–30% reoccur within 5 years even after surgery). - What is primary ciliary dyskinesia (PCD), and how does it relate to post-nasal drip?
PCD is a rare genetic disorder where cilia are dysmotile or immotile, preventing mucus clearance. Symptoms include chronic productive cough, post-nasal drip, recurrent sinusitis, and otitis media. Diagnosis involves nasal nitric oxide measurement (low in PCD) and ciliary beat frequency analysis. Treatment is supportive (regular saline irrigation, airway clearance). - Can laryngopharyngeal reflux (LPR) cause post-nasal drip sensation?
Yes. LPR occurs when stomach acid reaches the throat, triggering protective mucus production. Patients perceive this as post-nasal drip, throat clearing, or cough—often without classic heartburn. Treatment includes proton pump inhibitors (omeprazole), H2 blockers (ranitidine), and lifestyle modifications (avoid trigger foods, elevate bed head, no food 3 hours before sleep). - How does smoking affect nasal congestion and post-nasal drip?
Smoking damages ciliary epithelium, reducing ciliary beat frequency and impairing mucus clearance. Smokers experience worse nasal obstruction, post-nasal drip, and sinusitis. Additionally, passive smoke exposure increases risk in children. Quitting smoking significantly improves nasal symptoms and sinus disease outcomes. - Is there a role for long-term, low-dose antibiotics in chronic rhinosinusitis?
For select CRS patients, prolonged low-dose antibiotic courses (e.g., Azithromycin 250 mg 3x/week for 12 weeks) may provide benefit through anti-inflammatory effects, not just antibiotic action. However, evidence is mixed. Antibiotics are used judiciously after maximal medical therapy and are not standard first-line treatment. - What are the diagnostic criteria for chronic rhinosinusitis, and how is it confirmed?
Diagnosis requires BOTH:- Clinical: ≥12 weeks of symptoms (nasal obstruction, colored discharge, facial pain, or smell loss)AND Objective evidence: Endoscopy showing drainage/edema in middle meatus/anterior ethmoid, OR CT showing sinus inflammation
- Can nasal obstruction be related to sleep apnea, and should my ENT specialist screen for it?
Nasal obstruction is a risk factor for obstructive sleep apnea (OSA). Patients with moderate-severe nasal obstruction and symptoms (snoring, witnessed apneas, excessive daytime sleepiness) should be evaluated for OSA via sleep study. Treating nasal obstruction surgically can improve sleep apnea severity in some patients. - How soon should I see improvement after starting nasal steroid spray or saline rinse?
Saline rinse: Improvement may begin within hours (subjective relief) to days. Nasal steroids: Take 7–10 days for noticeable improvement; maximum effect at 2–4 weeks. If no improvement after 4 weeks of appropriate use, reassess diagnosis (imaging, allergy testing, specialist referral). Adherence and proper technique (Moffett’s position) are critical.
Hinglish FAQs — Sardi me Naak Band + Balgham (Post‑Nasal Drip)
- Post-nasal drip (PND) kya hota hai?
PND ka matlab hai naak ke peeche (nasopharynx) se mucus ka throat ke andar drip hona ya aisa feel hona ki “balgham gale me gir rahi hai”. - Kya PND normal cheez hai ya disease?
Thoda sa mucus nose se throat me naturally drain hota rehta hai, lekin jab mucus zyada ho, thick ho, ya drainage block ho to PND symptom ban jata hai. - Sardi me naak band kyun zyada hoti hai?
Winter me viral URTI (common cold) zyada hoti hai aur nasal mucosa inflamed ho jata hai, jis se obstruction aur discharge badhta hai. - Viral sinusitis aur bacterial sinusitis ka difference kaise samjhein?
Viral rhinosinusitis me symptoms <10 days aur worsening nahi hoti; ABRS tab suspect karte hain jab 10+ days me improvement na ho ya pehle better ho kar phir worse ho (double worsening). - “Double worsening / double sickening” kya hota hai?
Cold/sinus symptoms pehle 2–3 din better lagte hain, phir achanak phir se worsen ho jate hain—yeh ABRS suggest karta hai. - Kab antibiotics ki zarurat padti hai?
Agar symptoms 10 din se zyada persist kare bina improvement ke, ya double worsening ho, to ABRS suspect hota hai aur selected patients me antibiotics consider hoti hai. - Yellow/green mucus dikhe to kya hamesha bacterial hota hai?
Nahi. Purulent discharge viral/post-viral stage me bhi ho sakta hai; decision mainly duration (≥10 days), worsening pattern, fever, severe unilateral pain jaise criteria pe hota hai. - CRS (chronic rhinosinusitis) ka diagnosis kab hota hai?
Jab symptoms ≥12 weeks ho aur 2+ symptoms present ho (blockage/discharge essential) plus endoscopy/CT me inflammation ka proof mile. - CRS me kaunse symptoms common hote hain?
Nasal obstruction/congestion, nasal discharge (anterior ya posterior drip), facial pain/pressure, smell reduction/loss—इनमें se 2+ symptoms ≥12 weeks. - Saline nasal rinse / nasal douche kitna useful hai?
Saline irrigation CRS aur nasal symptoms me commonly recommended option hai; mucus, crusts aur irritants ko wash out karne me help karta hai. - Steam lena helpful hai ya myth?
EPOS 2020 me heated humidified air/steam ko common cold treatment me clear benefit nahi dikhaya gaya, isliye guaranteed “must do” nahi mana jata. - Nasal steroid spray (Fluticasone/Mometasone) kab use karna chahiye?
Acute post-viral rhinosinusitis me nasal corticosteroids total symptom score reduce kar sakte hain (effect small), aur CRS me long-term intranasal steroids effective aur safe maane jate hain. - Decongestant spray (Otrivin/Xylometazoline) kitne din use karein?
Short term use; guideline-based care pathways me decongestants <10 days ka mention hota hai, practical ENT practice me usually 3–5 din se zyada avoid kiya jata hai to rebound risk kam rahe. - LPR (silent reflux) se balgham kaise hoti hai?
LPR me throat me acid irritation hoti hai, body protective mucus banata hai; patient ko throat clearing aur “balgham” feel hoti hai. - DNS (deviated septum) se sardi me problem kyu badh jati hai?
DNS already airflow narrow karta hai; winter inflammation/rhinitis add ho jaye to obstruction aur blockage symptoms zyada prominent lagte hain (structural + inflammatory). - Nasal polyps me naak band aur smell loss kyu hota hai?
Polyps middle meatus/nasal cavity me obstruction create karte hain; EPOS criteria me polyps endoscopy ka objective evidence bhi hai. - Bachchon me unilateral badbu wali discharge ka matlab kya ho sakta hai?
Kids me unilateral foul-smelling discharge commonly nasal foreign body suggest karta hai—ENT evaluation needed. - Ek side se paani jaisi watery drip (especially jhukne par) dangerous ho sakti hai?
Haan, unilateral clear watery rhinorrhea (positional) CSF leak ka suspicion raise kar sakti hai—immediate ENT evaluation + imaging needed. - Eye swelling / double vision sinusitis me emergency kyu hai?
Periorbital edema/erythema, displaced globe, diplopia/ophthalmoplegia, reduced visual acuity EPOS “alarm symptoms” me aate hain—immediate referral required. - Hoarseness (awaz baith jana) >3 weeks ho to kya karna chahiye?
Persistent hoarseness 3+ weeks ENT evaluation demand karta hai, especially if PND/LPR symptoms bhi ho—laryngeal exam to rule out serious causes.
हिंदी FAQs — सर्दी में नाक बंद + बलगम (Post‑Nasal Drip)
- पोस्ट-नेज़ल ड्रिप (PND) क्या होता है?
PND का अर्थ है नाक के पीछे (नैसोफैरिंक्स) से स्राव का गले में पीछे की तरफ बहना या “बलगम गले में गिरने” जैसा महसूस होना. - क्या PND हमेशा बीमारी होती है?
नाक का थोड़ा स्राव सामान्य रूप से गले में जाता रहता है, लेकिन जब स्राव बहुत अधिक हो, बहुत गाढ़ा हो, या निकासी बाधित हो जाए, तब यह लक्षण बन जाता है. - सर्दियों में नाक ज़्यादा क्यों बंद होती है?
सर्दियों में वायरल URTI (कॉमन कोल्ड) अधिक होती है और नाक की झिल्ली में सूजन बढ़ती है, जिससे जकड़न और स्राव बढ़ता है. - वायरल और बैक्टीरियल साइनुसाइटिस में मुख्य फर्क क्या है?
वायरल राइनोसाइनुसाइटिस में लक्षण 10 दिनों से कम रहते हैं और लगातार बिगड़ते नहीं; ABRS तब माना जाता है जब 10+ दिनों में सुधार न हो या पहले सुधार के बाद फिर बिगड़ जाए (double worsening). - “डबल वर्सनिंग/डबल सिकनिंग” क्या होता है?
लक्षण पहले कुछ दिन बेहतर लगते हैं, फिर अचानक फिर से बिगड़ जाते हैं—यह बैक्टीरियल संक्रमण की संभावना बढ़ाता है. - एंटीबायोटिक कब ज़रूरी होती है?
जब 10 दिनों से अधिक समय तक लक्षण बिना सुधार के बने रहें या double worsening हो, तब चयनित मरीजों में एंटीबायोटिक पर विचार किया जाता है. - पीला/हरा बलगम दिखे तो क्या हमेशा बैक्टीरियल होता है?
नहीं। यह वायरल या पोस्ट-वायरल चरण में भी हो सकता है; निर्णय अवधि (≥10 दिन), लक्षणों के पैटर्न, बुखार, और एक तरफ़ का तेज दर्द जैसे मानदंडों पर होता है. - क्रॉनिक राइनोसाइनुसाइटिस (CRS) की परिभाषा क्या है?
CRS में लक्षण ≥12 हफ्ते रहते हैं और 2 या अधिक लक्षण होते हैं (नाक बंद होना/नाक से स्राव में से कम से कम एक), साथ में एंडोस्कोपी या CT पर सूजन का प्रमाण होना चाहिए. - CRS के मुख्य लक्षण कौन-कौन से हैं?
नाक बंद/जकड़न, नाक से स्राव (आगे या पीछे की तरफ), चेहरे में दबाव/दर्द, सूंघने की क्षमता कम होना—इनमें से 2+ लक्षण ≥12 हफ्ते. - नाक धोना (saline irrigation) कितना उपयोगी है?
EPOS में saline irrigation को विकल्प/समर्थित उपाय माना गया है; यह गाढ़े स्राव, क्रस्ट और इरिटेंट्स को धोकर निकालने में मदद कर सकता है. - भाप (steam) लेना ज़रूरी इलाज है?
EPOS 2020 में common cold के लिए heated, humidified air/steam से स्पष्ट लाभ नहीं मिला, इसलिए इसे “गारंटीड” इलाज नहीं माना जाता. - नाक का स्टेरॉयड स्प्रे कब उपयोग करें?
Acute post-viral rhinosinusitis में intranasal corticosteroids से कुल लक्षण स्कोर कुछ कम हो सकता है (प्रभाव छोटा), और CRS में लंबे समय तक इनका उपयोग प्रभावी व सुरक्षित माना गया है. - डीकन्जेस्टेंट स्प्रे (xylometazoline/oxymetazoline) कितने दिन?
Acute care pathways में decongestants <10 days दिया जाता है; प्रैक्टिकल ENT में आमतौर पर rebound से बचने हेतु 3–5 दिन से ज़्यादा नहीं रखने की सलाह दी जाती है. - LPR (silent reflux) से गले में बलगम क्यों लगता है?
LPR में गले में एसिड का रिफ्लक्स/इरिटेशन होता है, जिससे शरीर protective mucus बनाता है; मरीज को throat clearing और बलगम का एहसास होता है. - DNS (deviated septum) में सर्दी में समस्या क्यों बढ़ती है?
DNS से पहले से airflow कम होता है; सर्दी में rhinitis/सूजन जुड़ जाए तो obstruction ज्यादा महसूस होता है (structural + inflammatory). - नाक के पॉलिप्स में नाक बंद और सूंघने की समस्या क्यों?
पॉलिप्स nasal cavity/middle meatus में रुकावट बनाते हैं; EPOS criteria में nasal polyps objective evidence भी माने जाते हैं. - बच्चों में एक तरफ़ से बदबूदार स्राव आए तो क्या सोचें?
बच्चों में unilateral foul-smelling discharge अक्सर nasal foreign body का संकेत होता है—ENT evaluation जरूरी है. - एक तरफ़ से पानी जैसा स्राव (झुकने पर बढ़े) खतरनाक हो सकता है?
हाँ, unilateral clear watery rhinorrhea (positional) CSF leak का संदेह पैदा कर सकती है—immediate ENT evaluation और imaging जरूरी. - आंख की सूजन/डबल विज़न साइनुसाइटिस में emergency क्यों है?
Periorbital edema, displaced globe, double vision/ophthalmoplegia, reduced visual acuity EPOS के alarm symptoms हैं—immediate referral आवश्यक है. - आवाज़ बैठना (hoarseness) 3 हफ्ते से ज़्यादा रहे तो क्या करें?
3+ हफ्ते तक persistent hoarseness में ENT evaluation जरूरी है, खासकर अगर PND/LPR लक्षण साथ हों—laryngeal examination से गंभीर कारणों को exclude किया जाता है.
Secondary Keywords:
- Viral rhinosinusitis vs bacterial sinusitis
- Chronic rhinosinusitis (CRS) diagnosis
- Deviated nasal septum (DNS) surgery
- Nasal polyps causes and treatment
- Functional endoscopic sinus surgery (FESS)
- Septoplasty outcomes recovery
- Nasal douche alkaline wash technique
- Rhinitis medicamentosa rebound congestion
- Adenoid hypertrophy nasal blockage
- Laryngopharyngeal reflux LPR post-nasal drip
PRIME ENT Center Hardoi – Nasal Obstruction & Sinus Care
Address: PRIME ENT Center Hardoi, Hardoi 241001 (Uttar Pradesh), India
For Chronic Nasal Obstruction: Schedule Consultation / Endoscopic Evaluation
For Acute Sinusitis with High Fever/Facial Pain: Same-Day Assessment / Possible Imaging (CT)
For Suspected Deviated Septum: Endoscopic Assessment for Septoplasty Candidate Evaluation
What to Bring:
- Symptom duration and triggers
- Previous imaging (CT/MRI) if available
- Allergy testing results (if done)
- List of medications tried
Trust PRIME ENT Center Hardoi for Expert Management of Winter Nasal Symptoms and Chronic Rhinosinusitis
post nasal drip treatment, post nasal drip causes, naak band ka ilaaj, balgham gale me girna, winter nasal congestion, nasal blockage in winter, rhinitis vs sinusitis, acute rhinosinusitis symptoms, viral rhinosinusitis vs bacterial, acute bacterial rhinosinusitis criteria, double worsening sinusitis, facial pain pressure sinus, purulent nasal discharge, chronic rhinosinusitis 12 weeks, CRS symptoms EPOS, nasal saline irrigation, nasal douche kaise kare, alkaline nasal wash, nasal steroid spray fluticasone, mometasone nasal spray, decongestant spray 5 days rule, rhinitis medicamentosa rebound congestion, xylometazoline side effects, oxymetazoline rebound, vasomotor rhinitis cold air, non allergic rhinitis winter, allergic rhinitis indoor allergens, deviated nasal septum symptoms, DNS septoplasty, endoscopic septoplasty, turbinate hypertrophy treatment, turbinate reduction coblation, nasal polyps symptoms, ethmoidal polyps, antrochoanal polyp, chronic sinusitis with polyps, FESS for sinusitis, functional endoscopic sinus surgery, sinus CT scan when needed, nasal endoscopy CRS, adenoid hypertrophy mouth breathing, adenoidectomy for nasal blockage, laryngopharyngeal reflux mucus, LPR throat clearing, CSF leak watery discharge, unilateral nasal discharge foreign body, eye swelling sinus complication, ozaena atrophic rhinitis, crusting foul smell nose