Table of Contents
TL;DR – Quick Summary
Tree Pollen Allergy & Bagassosis in Winter-Spring:
- What it is: Seasonal allergic rhinitis from tree pollens (March-April peak) OR occupational bagassosis from sugarcane dust exposure during crushing season (December-May)
- Key difference from colds: Clear, watery discharge + intense itching/sneezing fits (allergy) vs. thick, discolored discharge + systemic illness (viral cold)
- Immune mechanism: Sensitized individuals produce IgE antibodies → mast cell degranulation within 5-15 minutes releases histamine → rapid onset symptoms
- Tree pollens affected: Holoptelea (65% in Jaipur), Eucalyptus, Gulmohar, Neem, Mango. Lightweight, windborne—penetrate homes
- Bagassosis risk: 92% of sugarcane mill workers exposed; 32-60% develop symptoms; 4.79x higher odds of chronic respiratory disease
- Treatment: Avoidance (HEPA filters, N95 masks) → nasal saline irrigation → nasal corticosteroid sprays → antihistamines → immunotherapy
- When to see ENT: Routine: persistent symptoms despite medications. Red flags: unilateral symptoms, severe dyspnea, failed therapy (4-6 weeks)
- Occupational protection: PPE reduces odds of chronic symptoms by 2.31x
English Version
Tree Pollen and Sugarcane Industry Allergy in Winter-Spring: Understanding Allergic Mechanisms, Recognizing Occupational Hazards, and Finding Effective Relief
Understanding tree pollen allergy and bagassosis (sugarcane dust allergy) is crucial for winter-spring respiratory health.As the harsh grip of mid-winter begins to loosen and early spring approaches, many individuals across India—from urban Hardoi to sugarcane-growing regions across Uttar Pradesh—experience a dramatic shift in respiratory health. While the common cold (viral rhinitis) dominates winter months, the winter-to-spring transition introduces distinct environmental and occupational triggers: windborne tree pollens and dust from sugarcane harvesting and milling operations.
At PRIME ENT Center Hardoi, Dr. Prateek Porwal and Dr. Harshita Singh frequently encounter patients who mistakenly attribute their symptoms to lingering infections when the true culprit is seasonal allergic rhinitis triggered by tree pollen exposure, or occupational bagassosis caused by sugarcane dust inhalation. Understanding these conditions, distinguishing them from infections, and implementing evidence-based management can dramatically improve quality of life during this transitional season.
The Seasonal Window: Tree Pollens in Winter-Spring Transition
Pollen Allergy Prevalence and Seasonality
Research indicates that pollen allergies affect approximately 40% of all allergic individuals globally, with significant regional variation based on local vegetation patterns. In India specifically:
- Pollen allergy affects 10–30% of adults and 20–25% of children
- Two major pollen seasons are documented: March–April (tree pollens) and August–October (grass/weed pollens)
- Tree pollens constitute the first peak of the pollen calendar year, often appearing as early as late January to February in some regions
Unlike summer’s grass and weed pollens, tree pollens are the earliest harbingers of allergy season. These pollens are:
- Lightweight and windborne: Travel easily through air, penetrating homes and workspaces despite closed windows
- Microscopic: Individual pollen grains measuring 15–100 micrometers settle on the nasal mucosa, initiating allergic responses in sensitized individuals
- Highly allergenic: Concentrated production ensures high atmospheric counts during flowering season
Major Tree Pollen Allergens in India:
Tree pollen surveys across India have identified diverse species:
- Holoptelea (major contributor in central India, particularly Jaipur region—up to 65% of pollen counts in March)
- Eucalyptus, Delonix regia (Gulmohar), Neem, Mango
- In northern regions: Chenopodiaceae, Poaceae families also significant
- Regional variation: Northern India higher incidence, North-Eastern states lower
Pollen Calendar for Central/Northern India:
- January–February: Low counts (winter harshness limits pollen production)
- March–April: Peak tree pollen season (major allergic rhinitis exacerbations)
- May–October: Grass and weed pollen seasons
Occupational Hazard: Bagassosis and Sugarcane Dust Exposure
The Occupational Context
For workers and residents in sugarcane-producing regions of India—notably Uttar Pradesh, Maharashtra, Karnataka, and Tamil Nadu—the winter-to-spring months (December–May) coincide with the active sugarcane crushing season. During this period, massive quantities of bagasse dust are generated.
What is Bagasse?
Bagasse is the fibrous residue remaining after juice extraction from sugarcane stalks. It is:
- Composed of cellulose fibers, typically 3–15 micrometers in diameter
- Stored in open or poorly ventilated facilities
- Often contaminated with fungal spores (Thermoactinomyces sacchari, Saccharopolyspora rectivirgula) and bacterial endotoxins
- Burned as biomass fuel in many mills, generating additional particulates and aerosols
Scale of Exposure
Evidence from India reveals alarming figures:
- 92% of sugarcane mill employees are exposed to bagasse dust [web:190]
- 32–60% of workers develop respiratory symptoms during active crushing seasons [web:190]
- 4.79 times higher odds of developing chronic respiratory symptoms with bagasse exposure (vs. non-exposed) [web:190]
- Symptoms resolve or reduce significantly during non-crushing seasons, confirming occupational causation
Bagassosis: The Disease
Bagassosis is a form of extrinsic allergic alveolitis (EAA)—a hypersensitivity pneumonitis caused by repeated inhalation of organic dust antigens.
Acute Bagassosis Presentation (4–8 hours post-exposure):
- High fever (38–40°C)
- Productive cough with expectoration of dark mucus
- Shortness of breath (dyspnea) and chest tightness
- Malaise and fatigue
- No wheezing (distinguishing from asthma initially)
Chronic Bagassosis (repeated exposure over months/years):
- Insidious progressive dyspnea
- Persistent productive cough
- Recurrent respiratory infections
- Reduced exercise tolerance
- Progressive lung fibrosis on imaging (worst case)
Upper Airway Involvement:
While bagassosis primarily affects lower airways and alveoli, initial exposure often involves upper airway irritation: nasal congestion, nasal discharge, throat irritation, and cough.
The Immune Mechanism: Understanding Allergic Sensitization and Response
To understand why certain individuals develop allergies to tree pollen or bagasse dust while others do not, one must understand the immunologic cascade.
Stage 1: Sensitization (First Exposure)
Upon initial exposure to an allergen (tree pollen or bagasse dust), in genetically predisposed individuals:
- Antigen Presentation: Dendritic cells (specialized immune cells) capture pollen grains or dust particles in the nasal mucosa
- T Cell Activation: These dendritic cells migrate to lymph nodes, presenting the allergen to naive T helper cells (Th0)
- Th2 Polarization: IL-4 and IL-13 (cytokines) drive differentiation toward Th2 cells (pro-allergic profile)
- B Cell Activation: Activated Th2 cells stimulate B cells through CD40-CD154 interaction
- IgE Production: B cells undergo class-switch recombination, producing allergen-specific IgE antibodies [web:191][web:194]
Critical Point: Sensitization occurs silently—the individual may have no symptoms during first exposure.
Stage 2: Re-exposure and Early-Phase Response (Minutes)
Upon subsequent exposure to the same allergen in a sensitized individual:
- IgE Binding: Allergen-specific IgE antibodies (produced during sensitization) are bound to high-affinity IgE receptors (FcεRI) on mast cell surfaces in nasal mucosa and basophil surfaces in blood
- Cross-Linking: Allergen binds to and cross-links these IgE molecules on mast cells
- Mast Cell Degranulation: Within 5–15 minutes, mast cells release preformed mediators:
- Histamine (primary mediator, causes itching, sneezing, vasodilation)
- Proteases and tryptase (tissue damage)
- Leukotrienes (LTC4, LTD4, LTE4) (cause bronchoconstriction, mucus secretion)
- Prostaglandins (PGD2) (vasodilation, secretion)
- Platelet-activating factor (PAF)
Result: Rapid onset of symptoms—sneezing, nasal itching, watery rhinorrhea, and congestion
Stage 3: Late-Phase Response (4–10 Hours)
Hours after allergen exposure:
- Cytokine Release: Activated mast cells secrete IL-4, IL-5, IL-13, TNF-α, GM-CSF
- Inflammatory Cell Recruitment: These cytokines recruit:
- Eosinophils (produce major basic protein, cause tissue inflammation)
- T cells (further amplify Th2 response)
- Basophils (additional histamine release)
- Neutrophils (tissue damage)
- Adhesion Molecule Expression: Endothelial cells upregulate ICAM-1 and VCAM-1, enhancing cell migration into nasal tissue
- Mucosal Edema: Vascular leak and fluid accumulation cause nasal swelling and congestion
Result: Persistent nasal obstruction, discharge, and symptoms lasting hours to days
Why Some People Are More Susceptible:
Genetic and environmental factors predispose to allergic sensitization:
- Genetic predisposition: Family history of atopy (asthma, eczema, allergic rhinitis)
- Early-life exposures: Timing and intensity of allergen exposure during critical immune windows
- IL-33 polymorphisms: Recent studies show specific IL-33 gene variants linked to allergic rhinitis (particularly in Han Chinese population, likely relevant in other Asian populations)
- Environmental cofactors: Air pollution, smoking exposure, diesel exhaust particles enhance allergic sensitization
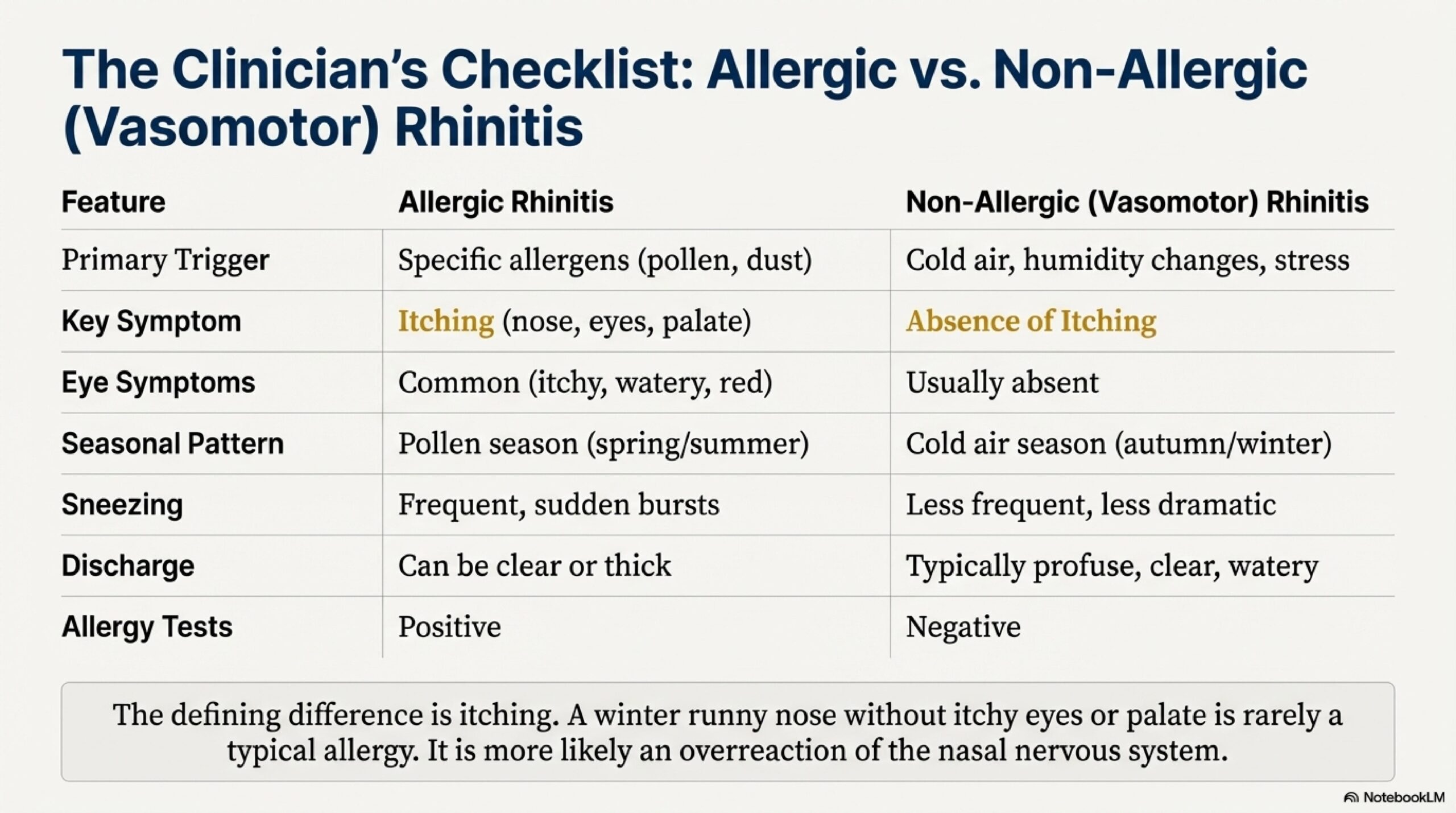
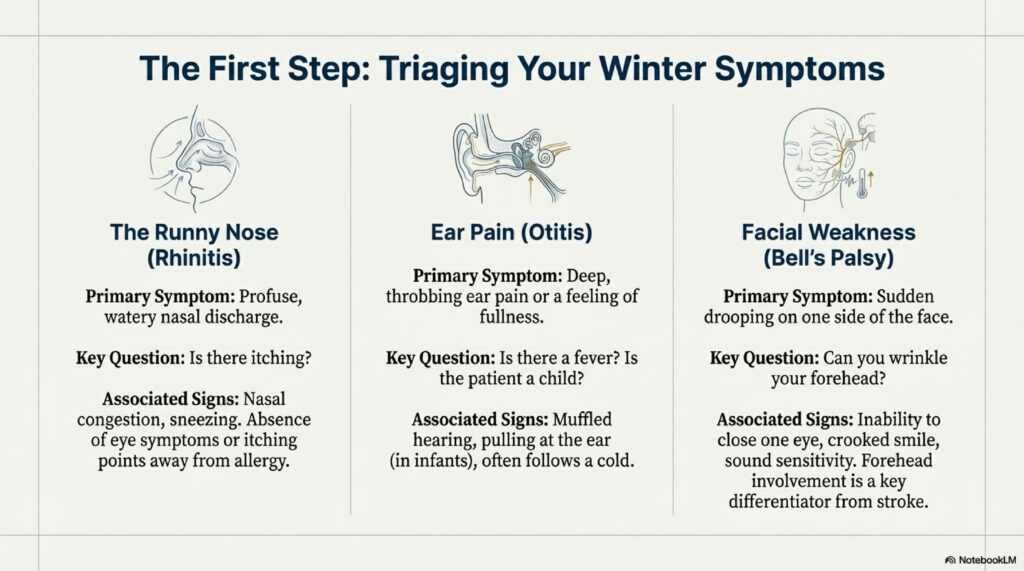
Symptoms and Signs: Distinguishing Allergy from Infection
Cardinal Features of Allergic Rhinitis (Seasonal)
Unlike the thick, discolored discharge of viral rhinitis, seasonal allergic rhinitis presents distinctively:
Nasal Symptoms:
- Frequent, paroxysmal sneezing: Often explosive, in “sneezing fits” of 5–10+ consecutive sneezes
- Nasal itching (pruritus): Often intense, driving patient to rub nose repeatedly
- Clear, watery rhinorrhea: Profuse anterior nasal discharge
- Nasal obstruction/congestion: Due to mucosal edema (late-phase), often bilateral and alternating
Ocular Symptoms (Allergic Conjunctivitis):
- Red, itchy, watery eyes
- Chemosis (conjunctival swelling)
- Photophobia (light sensitivity) in severe cases
Physical Signs in Children (Pathognomonic):
- Allergic salute: Repeated upward rubbing of nose with open palm, often leaving a transverse crease across the bridge of nose (called “Dennie’s crease“)
- Allergic shiners: Dark circles under eyes (from venous congestion in lower lid)
- Open mouth posture: Chronic mouth breathing due to nasal obstruction
- “Adenoid facies”: If prolonged, can develop dental malocclusion
Respiratory Symptoms (From Bagasse Exposure):
- Nasal symptoms (as above) plus
- Productive cough with clear, watery, or slightly blood-tinged sputum
- Wheezing (in bagassosis cases or those with concurrent asthma)
- Dyspnea (shortness of breath) on exertion or at rest (severe cases)
- Fever (in acute bagassosis exposure)
Key Differentiating Features:
| Feature | Allergic Rhinitis | Viral Rhinitis (Cold) |
|---|---|---|
| Discharge | Clear, watery | Thick, yellowish/green |
| Itching | Prominent | Minimal |
| Sneezing | Paroxysmal fits | Mild |
| Onset | Acute (upon exposure) | Gradual (1–3 days) |
| Duration | Continues while exposed | Self-limited 7–14 days |
| Fever | Absent (unless bagassosis) | Present (usually) |
| Systemic Symptoms | Absent | Malaise, fatigue |
Management and Relief Strategies
Primary Management Goals:
- Avoid/minimize allergen exposure
- Reduce inflammatory response
- Stabilize mast cells to prevent degranulation
- Symptomatic relief
- For occupational exposures, implement workplace protections
A. Environmental Control and Allergen Avoidance
Pollen Avoidance (Non-Occupational Settings):
- Keep windows closed during peak pollen season (March–April)
- Use HEPA filtration: Home air purifiers with HEPA filters reduce indoor pollen by 85–95%
- Wear pollen-rated masks outdoors (N95, KN95 masks effective; specialized pollen masks available)
- Wash face and hair after outdoor exposure to remove settled pollen
- Change clothes and shower after outdoor activities
- Dry laundry indoors (outdoor clotheslines collect pollen)
- Car air filters: Use cabin air filters (preferably HEPA-rated) in vehicles
Occupational Protection (Sugarcane Workers):
- High-filtration respiratory masks (N95/FFP2 minimum): During crushing season, especially during high-dust activities (bagasse handling, transport)
- Full personal protective equipment (PPE): Face shield, eye protection, protective clothing
- Workplace engineering controls: Local exhaust ventilation at dust generation sources, wet suppression (wetting bagasse to reduce airborne particles)
- Education and compliance: Worker awareness of hazards, proper mask fit testing, training on PPE use
- Regular health screening: Baseline and periodic spirometry (lung function testing) for workers to detect early airflow obstruction
Regulatory Note: Research shows workers with proper respiratory protection had 2.31 times lower odds of developing chronic respiratory symptoms compared to those without PPE [web:190].
B. Nasal Saline Irrigation (Douching)
As discussed in the previous nasal obstruction article, alkaline nasal douching is a cornerstone:
- Solution: Warm isotonic (0.9%) or hypertonic (2.3%) saline + baking soda + sodium biborate
- Frequency: 1–2 times daily, especially after outdoor exposure
- Benefit: Mechanically removes pollen and dust, prevents prolonged mucosal contact, reduces symptom severity
C. Pharmacotherapy
1. Antihistamines (First-Line for Allergic Rhinitis)
Second-Generation (Preferred):
- Non-sedating, minimal blood-brain barrier penetration
- Cetirizine (Piriteze, Alleroff): 10 mg daily, very effective, minimal sedation
- Loratadine (Claritin): 10 mg daily, minimal sedation
- Fexofenadine (Allegra): 120–180 mg daily, minimal sedation
- Desloratadine: 5 mg daily, potent
First-Generation (Older, Less Preferred):
- Cause sedation, anticholinergic effects
- Examples: Chlorpheniramine, diphenhydramine (now rarely used for allergic rhinitis)
Onset and Duration: Second-generation antihistamines take 30–60 minutes for onset; maximum effect at 1–2 weeks with regular use. Most effective when started before pollen season begins (prophylactic use).
2. Topical Nasal Corticosteroids (Most Effective Long-Term)
Mechanism: Reduce mucosal edema, inhibit mast cell degranulation, reduce cytokine production
Recommended Agents:
- Fluticasone propionate (Flovent, Nasalide): 50 micrograms/spray, 1–2 sprays per nostril daily
- Mometasone (Nasonex): 50 micrograms/spray, 1–2 sprays per nostril daily
- Triamcinolone: 55 micrograms/spray
- Ciclesonide: Prodrug (activated in nasal tissue, minimal systemic absorption)
Application (Critical): Use Moffett’s position (head tilted forward and down) to ensure medicine reaches posterior nasal cavity and sinuses
Efficacy: 60–80% experience significant symptom improvement within 1–2 weeks; maximum benefit at 4 weeks
Safety: Minimal systemic absorption (especially ciclesonide); safe for long-term use (months to years)
3. Cromolyn Sodium (Mast Cell Stabilizer)
Mechanism: Prevents mast cell degranulation by stabilizing cell membranes
Administration: Nasal spray, 5.2 mg per spray, 1 spray each nostril 3–4 times daily
Advantage: Highly effective for prophylaxis (prevention)—must be started before allergen exposure
Disadvantage: Less effective than antihistamines or steroids for established symptoms; requires frequent dosing
Use Case: Ideal for individuals aware of upcoming allergen exposure (e.g., planning outdoor activities during high pollen season)
4. Anticholinergics (For Profuse Watery Rhinorrhea)
Ipratropium Bromide (Atrovent nasal spray): 21 micrograms per spray, 2 sprays per nostril 2–3 times daily
Mechanism: Blocks muscarinic receptors on mucous glands, reducing secretion
Particularly Effective For: Vasomotor rhinitis (non-allergic) and severe watery rhinorrhea in allergic rhinitis
Benefit: Doesn’t cause systemic anticholinergic side effects (minimal absorption)
D. Immunotherapy (SCIT/SLIT)
For patients with persistent, severe symptoms not controlled by medications, or those sensitized to multiple seasonal allergens:
Subcutaneous Immunotherapy (SCIT or “Allergy Shots”):
- Gradual administration of increasing allergen extract concentrations
- Builds IgG-blocking antibodies that compete with IgE for allergen binding
- Induces immune tolerance (T regulatory cell formation)
- Duration: 3–5 years treatment followed by clinical benefit lasting years
- Efficacy: 60–90% symptom improvement
Sublingual Immunotherapy (SLIT or “Allergy Tablets”):
- Allergen tablets dissolved under tongue
- More convenient than injections, fewer systemic reactions
- Similar efficacy to SCIT
- Examples: Grass pollen tablets (Oralair, Grastek), dust mite tablets (Acarizax)
Indications:
- Multiple seasonal allergens
- Severe symptoms
- Failure of maximal medical therapy
- Desire for long-term curative solution
When to Seek ENT Specialist Evaluation
Routine Evaluation (1–2 Days):
- Persistent sneezing and nasal itching despite antihistamines
- Nasal obstruction limiting quality of life despite nasal steroids
- Watery rhinorrhea affecting work/sleep
- Symptoms spanning multiple seasons suggesting polysensitization
Same-Day Evaluation (Red Flags):
- Unilateral symptoms: Blockage or discharge only on one side (suggests structural problem, not allergy)
- Severe dyspnea or wheezing: Suggest asthma exacerbation or bagassosis progression
- Failed medical therapy (4–6 weeks): May need endoscopy, imaging, or immunotherapy assessment
- Occupational exposure with progressive symptoms: Suggest spirometry, chest imaging to assess for bagassosis
The “Filter and Flue” Analogy: Understanding Winter-Spring Allergies
Dr. Harshita Singh uses this analogy with patients:
“Think of your respiratory system as a high-end fireplace with a sophisticated flue (nasal passages and sinuses). In summer, the air is clean and the flue is open—no problems. When winter turns to spring, the ‘ash’ (tree pollen) and ‘soot’ (sugarcane dust) begin to fly in the wind. If your ‘chimney filter’ (nasal mucosa) is over-sensitive—perhaps genetically programmed to over-react to these harmless particles—it swells and closes shut. This causes ‘smoke’ (inflammation) to billow back into the ‘room’ (your lungs and sinuses), making you miserable.
Treatment is like maintaining your fireplace:
- Saline washes act like a broom to sweep out the soot and ash before they stick
- Steroid sprays act like a cooling agent to prevent the chimney from over-reacting and swelling shut
- Antihistamines block the inflammatory cascade that causes the swelling
- Cromolyn acts like a preventive coating to stop particles from triggering the reaction
- If the flue itself is bent or damaged (like a truly deviated septum or airway blockage), a surgeon may need to straighten it
By managing the environmental ‘soot’ and ‘ash’ early, and quieting the over-reactive immune response, you keep your whole respiratory system breathing easily.”
Hinglish Version
Sardi me Tree Pollen aur Sugarcane Industry Allergy: Winter-Spring Transition
Jab sardi ka kahanah loose hota hai aur spring approach karta hai, many individuals ko respiratory health suddenly worse ho jati है। Common cold (viral) winter mein prevalent hota है, lekin winter-to-spring transition mein distinct environmental aur occupational triggers introduce hote हैं: windborne tree pollens aur sugarcane dust।
PRIME ENT Center Hardoi mein, Dr. Prateek Porwal aur Dr. Harshita Singh frequently dekha karte हैं patients jo गलती से think करते हैं कि lingering infection है, जबकि असल में seasonal allergic rhinitis है या bagassosis (sugarcane occupational allergy)।
Seasonal Window: Tree Pollens
Prevalence:
- Pollen allergy ~40% of allergic individuals को affect करता है worldwide [web:186]
- India में: 10-30% adults, 20-25% children [web:187]
- Two major peaks: March-April (tree), August-October (grass/weed) [web:189]
Tree Pollens:
- Lightweight, windborne, microscopic
- 15-100 micrometers size
- Close windows mein bhi enter kar जाते हैं
- Early season (Jan-Feb in some regions)
Major Trees in India:
- Holoptelea (65% in Jaipur region, March peak) [web:189]
- Eucalyptus, Gulmohar, Neem, Mango
- Regional variation: North India higher, Northeast lower [web:187]
Occupational Hazard: Bagassosis aur Sugarcane Dust
Bagasse Kya Hai:
- Sugarcane का fibrous residue (juice extract करने के बाद)
- 3-15 micrometer fibers
- Open/poor ventilation में stored
- Fungal spores से contaminated (Thermoactinomyces sacchari, Saccharopolyspora rectivirgula) [web:193]
- Burned as biomass fuel—additional particles generate होते हैं
Scale in India:
- 92% sugarcane mill workers bagasse dust expose हो जाते हैं [web:190]
- 32-60% workers active crushing season mein respiratory symptoms develop करते हैं [web:190]
- 4.79 times higher odds chronic respiratory symptoms का (bagasse exposure से) [web:190]
- Symptoms resolve non-crushing season mein—occupational causation confirm होता है [web:190]
Bagassosis: Disease
- Extrinsic allergic alveolitis (EAA) form
- Repeated inhalation से organic dust antigens
Acute (4-8 hours post-exposure):
- High fever (38-40°C)
- Productive cough (dark mucus)
- Dyspnea, chest tightness
- Malaise, fatigue
Chronic (months/years repeated):
- Progressive dyspnea
- Persistent cough
- Recurrent infections
- Reduced exercise tolerance
- Lung fibrosis (worst case)
Upper Airway Involvement: Nasal congestion, discharge, throat irritation, cough
Immune Mechanism: Sensitization aur Allergic Response
Stage 1: Sensitization (First Exposure)
Genetically predisposed लोगों में:
- Antigen Presentation: Dendritic cells capture pollen/dust nasal mucosa में
- T Cell Activation: Nasal lymph nodes में Th0 को present करते हैं
- Th2 Polarization: IL-4, IL-13 से Th2 differentiation (pro-allergic)
- B Cell Activation: Th2 cells activate B cells (CD40-CD154 interaction)
- IgE Production: B cells करते हैं allergen-specific IgE antibodies produce [web:191][web:194]
Key: Sensitization silent होता है—first exposure पर कोई symptoms नहीं।
Stage 2: Re-exposure, Early-Phase (Minutes)
Subsequent exposure में:
- IgE Binding: Allergen-specific IgE bound होते हैं high-affinity receptors (FcεRI) पर mast cells (nasal mucosa) aur basophils (blood)
- Cross-Linking: Allergen cross-links ये IgE molecules
- Mast Cell Degranulation: 5-15 minutes में preformed mediators release:
- Histamine (itching, sneezing, vasodilation)
- Proteases, tryptase (tissue damage)
- Leukotrienes (LTC4, LTD4) (bronchospasm, mucus secretion)
- Prostaglandins (PGD2) (vasodilation)
- Platelet-activating factor (PAF)
Result: Rapid symptoms—sneezing, nasal itching, watery rhinorrhea, congestion
Stage 3: Late-Phase (4-10 Hours)
- Cytokine Release: Mast cells secrete IL-4, IL-5, IL-13, TNF-α
- Inflammatory Cell Recruitment:
- Eosinophils
- T cells
- Basophils
- Neutrophils
- Adhesion Molecules: Endothelial cells upregulate ICAM-1, VCAM-1
- Mucosal Edema: Vascular leak, fluid accumulation
Result: Persistent obstruction, discharge
Susceptibility Factors:
- Genetic predisposition (family history)
- Early-life allergen exposures
- IL-33 gene polymorphisms
- Air pollution, smoking, diesel exhaust
Symptoms aur Signs
Allergic Rhinitis (Seasonal):
Nasal:
- Paroxysmal sneezing (5-10+ consecutive)
- Nasal itching (pruritus) intense
- Clear, watery rhinorrhea (profuse)
- Nasal obstruction bilateral, alternating
Ocular (Allergic Conjunctivitis):
- Red, itchy, watery eyes
- Chemosis
- Photophobia (severe cases)
Physical Signs in Children:
- Allergic salute: Upward rubbing nose→transverse crease (Dennie’s crease)
- Allergic shivers: Dark circles under eyes (venous congestion)
- Open mouth posture
- Adenoid facies (prolonged)
Respiratory (Bagasse Exposure):
- Nasal symptoms + productive cough (clear/watery/blood-tinged)
- Wheezing
- Dyspnea
- Fever (acute bagassosis)
Differentiating:
| Feature | Allergic | Viral (Cold) |
|---|---|---|
| Discharge | Clear, watery | Thick, yellow/green |
| Itching | Prominent | Minimal |
| Sneezing | Paroxysmal fits | Mild |
| Onset | Acute (upon exposure) | Gradual (1-3 days) |
| Duration | While exposed | 7-14 days |
| Fever | Absent (unless bagassosis) | Usually present |
| Systemic | Absent | Malaise, fatigue |
Management aur Relief
Goals:
- Allergen avoidance
- Reduce inflammation
- Stabilize mast cells
- Symptomatic relief
- Occupational protection (workers)
A. Environmental Control
Pollen Avoidance:
- Windows close (March-April peak)
- HEPA filters: 85-95% pollen reduction
- Pollen-rated masks outdoors (N95, KN95)
- Face/hair wash after outdoor time
- Change clothes, shower
- Indoor laundry drying
- Car HEPA filters
Occupational (Sugarcane Workers):
- N95/FFP2 masks minimum (crushing season especially)
- Full PPE: Face shield, eye protection, protective clothing
- Workplace controls: Local exhaust ventilation, wet suppression (water spray reduce dust)
- Education: Worker awareness, mask fit testing, training
- Health screening: Baseline spirometry, periodic tests (detect early airflow obstruction)
- Research shows proper PPE से 2.31 times lower odds chronic symptoms [web:190]
B. Nasal Saline Irrigation
- Solution: Warm isotonic (0.9%) या hypertonic (2.3%) + baking soda + sodium biborate
- Frequency: 1-2x daily, especially after outdoor
- Benefit: Mechanically removes pollen/dust, reduces mucosal contact, lowers symptoms
C. Pharmacotherapy
1. Antihistamines (First-Line)
Second-Generation (Preferred):
- Non-sedating, minimal BBB penetration
- Cetirizine (Piriteze): 10 mg daily
- Loratadine (Claritin): 10 mg daily
- Fexofenadine (Allegra): 120-180 mg daily
- Desloratadine: 5 mg daily
Onset: 30-60 minutes; max effect 1-2 weeks regular use
Best: Start before season (prophylactic)
2. Nasal Corticosteroids (Most Effective Long-Term)
- Fluticasone: 50 micrograms/spray, 1-2 daily
- Mometasone (Nasonex): 50 micrograms/spray, 1-2 daily
- Triamcinolone: 55 micrograms/spray
- Ciclesonide: Prodrug (minimal systemic)
Application: Moffett’s position (head forward/down)
Efficacy: 60-80% improvement 1-2 weeks; max 4 weeks
Safety: Minimal systemic—safe long-term
3. Cromolyn Sodium (Mast Cell Stabilizer)
- Nasal spray, 5.2 mg/spray
- 1 spray per nostril, 3-4x daily
- Prophylaxis के लिए ideal (must start before exposure)
- Less effective for established symptoms; frequent dosing
4. Anticholinergics
- Ipratropium (Atrovent): 21 micrograms/spray, 2 sprays TID
- Blocks mucous gland secretion
- Particularly for watery rhinorrhea (vasomotor या allergic severe)
- Minimal systemic effects
D. Immunotherapy (SCIT/SLIT)
For persistent, severe symptoms या multiple allergen sensitization:
SCIT (Allergy Shots):
- Gradual increasing allergen concentrations
- Builds IgG-blocking antibodies
- Induces immune tolerance (T regulatory cells)
- Duration: 3-5 years, then benefit lasts years
- Efficacy: 60-90%
SLIT (Allergy Tablets):
- Allergen tablets under tongue
- Convenient, fewer systemic reactions
- Similar efficacy to SCIT
- Examples: Grass (Oralair), dust mite (Acarizax)
Kab Doctor Dikhao
1-2 दिनों में:
- Persistent sneezing/itching despite antihistamines
- Obstruction limiting life despite steroids
- Watery rhinorrhea affecting sleep
- Multi-season symptoms
Same-Day (Red Flags):
- Unilateral symptoms (one side only)—suggests structural, not allergy
- Severe dyspnea/wheezing—asthma exacerbation or bagassosis
- Failed therapy (4-6 weeks)—endoscopy/imaging/immunotherapy assess
- Occupational progressive symptoms—spirometry, chest imaging (bagassosis screening)
हिंदी संस्करण
सर्दी में Tree Pollen और Sugarcane Industry Allergy: Winter-Spring Transition
जब सर्दी का कहर ढीला होता है और वसंत (spring) पास आता है, कई लोगों को respiratory health अचानक बदतर हो जाती है। Common cold (वायरल) सर्दियों में प्रचलित होता है, लेकिन winter-to-spring transition में distinct environmental और occupational triggers होते हैं: tree pollens और sugarcane dust।
PRIME ENT Center Hardoi में, डॉ प्रतीक पोरवाल और डॉ हर्षिता सिंह अक्सर ऐसे मरीजों को देखते हैं जो गलत तरीके से सोचते हैं कि lingering infection है, जबकि असल में seasonal allergic rhinitis या bagassosis (sugarcane occupational allergy) है।
Seasonal Window: Tree Pollens
Prevalence:
- Pollen allergy ~40% allergic individuals को affect करता है worldwide [web:186]
- भारत में: 10-30% adults, 20-25% children [web:187]
- दो मुख्य पीक: March-April (tree), August-October (grass/weed) [web:189]
Tree Pollens:
- Lightweight, windborne, microscopic
- 15-100 micrometers आकार
- Close windows में भी enter हो जाते हैं
- Early season (कुछ regions में Jan-Feb)
भारत में मुख्य पेड़:
- Holoptelea (Jaipur में 65%, March peak) [web:189]
- Eucalyptus, Gulmohar, Neem, Mango
- Regional variation: North higher, Northeast lower [web:187]
Occupational Hazard: Bagassosis और Sugarcane Dust
Bagasse क्या है:
- Sugarcane का fibrous residue (juice निकालने के बाद)
- 3-15 micrometer fibers
- Open/poorly ventilated में stored
- Fungal spores से contaminated (Thermoactinomyces sacchari, Saccharopolyspora rectivirgula) [web:193]
- Biomass fuel के रूप में जलाया जाता है—अतिरिक्त particles generate होते हैं
भारत में Scale:
- 92% sugarcane mill workers bagasse dust exposure [web:190]
- 32-60% workers active crushing season में respiratory symptoms develop करते हैं [web:190]
- 4.79 times higher odds chronic respiratory symptoms का (bagasse exposure से) [web:190]
- Symptoms resolve non-crushing season में—occupational causation confirm होता है [web:190]
Bagassosis: बीमारी
- Extrinsic allergic alveolitis (EAA) form
- Repeated inhalation से organic dust antigens
Acute (4-8 hours post-exposure):
- High fever (38-40°C)
- Productive cough (dark mucus)
- Dyspnea, chest tightness
- Malaise, fatigue
Chronic (महीनों/सालों repeated):
- Progressive dyspnea
- Persistent cough
- Recurrent infections
- Reduced exercise tolerance
- Lung fibrosis (worst case)
Upper Airway Involvement: Nasal congestion, discharge, throat irritation, cough
Immune Mechanism: Sensitization और Allergic Response
Stage 1: Sensitization (First Exposure)
Genetically predisposed लोगों में:
- Antigen Presentation: Dendritic cells capture pollen/dust nasal mucosa में
- T Cell Activation: Nasal lymph nodes में Th0 को present करते हैं
- Th2 Polarization: IL-4, IL-13 से Th2 differentiation (pro-allergic)
- B Cell Activation: Th2 cells activate B cells (CD40-CD154 interaction)
- IgE Production: B cells allergen-specific IgE antibodies produce करते हैं [web:191][web:194]
Key: Sensitization silent होता है—first exposure पर कोई symptoms नहीं।
Stage 2: Re-exposure, Early-Phase (Minutes)
Subsequent exposure में:
- IgE Binding: Allergen-specific IgE bound होते हैं high-affinity receptors (FcεRI) पर mast cells (nasal mucosa) और basophils (blood)
- Cross-Linking: Allergen cross-links ये IgE molecules
- Mast Cell Degranulation: 5-15 minutes में preformed mediators release:
- Histamine (itching, sneezing, vasodilation)
- Proteases, tryptase (tissue damage)
- Leukotrienes (LTC4, LTD4) (bronchospasm, mucus secretion)
- Prostaglandins (PGD2) (vasodilation)
- Platelet-activating factor (PAF)
Result: Rapid symptoms—sneezing, nasal itching, watery rhinorrhea, congestion
Stage 3: Late-Phase (4-10 Hours)
- Cytokine Release: Mast cells secrete IL-4, IL-5, IL-13, TNF-α
- Inflammatory Cell Recruitment:
- Eosinophils
- T cells
- Basophils
- Neutrophils
- Adhesion Molecules: Endothelial cells upregulate ICAM-1, VCAM-1
- Mucosal Edema: Vascular leak, fluid accumulation
Result: Persistent obstruction, discharge
Susceptibility Factors:
- Genetic predisposition (family history)
- Early-life allergen exposures
- IL-33 gene polymorphisms
- Air pollution, smoking, diesel exhaust
Symptoms और Signs
Allergic Rhinitis (Seasonal):
Nasal:
- Paroxysmal sneezing (5-10+ consecutive)
- Nasal itching (pruritus) intense
- Clear, watery rhinorrhea (profuse)
- Nasal obstruction bilateral, alternating
Ocular (Allergic Conjunctivitis):
- Red, itchy, watery eyes
- Chemosis
- Photophobia (severe cases)
Physical Signs in Children:
- Allergic salute: Upward nose rubbing→transverse crease (Dennie’s crease)
- Allergic shiners: Dark circles under eyes (venous congestion)
- Open mouth posture
- Adenoid facies (prolonged)
Respiratory (Bagasse Exposure):
- Nasal symptoms + productive cough (clear/watery/blood-tinged)
- Wheezing
- Dyspnea
- Fever (acute bagassosis)
Differentiating:
| Feature | Allergic | Viral (Cold) |
|---|---|---|
| Discharge | Clear, watery | Thick, yellow/green |
| Itching | Prominent | Minimal |
| Sneezing | Paroxysmal fits | Mild |
| Onset | Acute (upon exposure) | Gradual (1-3 दिन) |
| Duration | While exposed | 7-14 दिन |
| Fever | Absent (unless bagassosis) | Usually present |
| Systemic | Absent | Malaise, fatigue |
Management और Relief
Goals:
- Allergen avoidance
- Reduce inflammation
- Stabilize mast cells
- Symptomatic relief
- Occupational protection (workers)
A. Environmental Control
Pollen Avoidance:
- Windows close (March-April peak)
- HEPA filters: 85-95% pollen reduction
- Pollen-rated masks outdoors (N95, KN95)
- Face/hair wash after outdoor
- Change clothes, shower
- Indoor laundry drying
- Car HEPA filters
Occupational (Sugarcane Workers):
- N95/FFP2 masks minimum (crushing season especially)
- Full PPE: Face shield, eye protection, protective clothing
- Workplace controls: Local exhaust ventilation, wet suppression (water spray dust reduce करता है)
- Education: Worker awareness, mask fit testing, training
- Health screening: Baseline spirometry, periodic tests (early airflow obstruction detect करने के लिए)
- Research दिखाता है proper PPE से 2.31 times lower odds chronic symptoms [web:190]
B. Nasal Saline Irrigation
- Solution: Warm isotonic (0.9%) या hypertonic (2.3%) + baking soda + sodium biborate
- Frequency: 1-2x daily, especially after outdoor
- Benefit: Mechanically removes pollen/dust, reduces mucosal contact, lowers symptoms
C. Pharmacotherapy
1. Antihistamines (First-Line)
Second-Generation (Preferred):
- Non-sedating, minimal BBB penetration
- Cetirizine (Piriteze): 10 mg daily
- Loratadine (Claritin): 10 mg daily
- Fexofenadine (Allegra): 120-180 mg daily
- Desloratadine: 5 mg daily
Onset: 30-60 minutes; max effect 1-2 weeks regular use
Best: Start before season (prophylactic)
2. Nasal Corticosteroids (Most Effective Long-Term)
- Fluticasone: 50 micrograms/spray, 1-2 daily
- Mometasone (Nasonex): 50 micrograms/spray, 1-2 daily
- Triamcinolone: 55 micrograms/spray
- Ciclesonide: Prodrug (minimal systemic)
Application: Moffett’s position (head forward/down)
Efficacy: 60-80% improvement 1-2 weeks; max 4 weeks
Safety: Minimal systemic—safe long-term
3. Cromolyn Sodium (Mast Cell Stabilizer)
- Nasal spray, 5.2 mg/spray
- 1 spray per nostril, 3-4x daily
- Prophylaxis के लिए ideal (must start before exposure)
- Less effective established symptoms के लिए; frequent dosing
4. Anticholinergics
- Ipratropium (Atrovent): 21 micrograms/spray, 2 sprays TID
- Blocks mucous gland secretion
- Particularly for watery rhinorrhea (vasomotor या allergic severe)
- Minimal systemic effects
D. Immunotherapy (SCIT/SLIT)
For persistent, severe symptoms या multiple allergen sensitization:
SCIT (Allergy Shots):
- Gradual increasing allergen concentrations
- Builds IgG-blocking antibodies
- Induces immune tolerance (T regulatory cells)
- Duration: 3-5 years, then benefit lasts years
- Efficacy: 60-90%
SLIT (Allergy Tablets):
- Allergen tablets under tongue
- Convenient, fewer systemic reactions
- Similar efficacy to SCIT
- Examples: Grass (Oralair), dust mite (Acarizax)
कब Doctor दिखाएं
1-2 दिनों में:
- Persistent sneezing/itching despite antihistamines
- Obstruction limiting life despite steroids
- Watery rhinorrhea affecting sleep
- Multi-season symptoms
Same-Day (Red Flags):
- Unilateral symptoms (एक side only)—suggests structural, not allergy
- Severe dyspnea/wheezing—asthma exacerbation या bagassosis
- Failed therapy (4-6 weeks)—endoscopy/imaging/immunotherapy assess
- Occupational progressive symptoms—spirometry, chest imaging (bagassosis screening)
FAQ: English Version
20 Frequently Asked Questions About Tree Pollen Allergy and Bagassosis
- What is the difference between seasonal allergic rhinitis triggered by pollen and a lingering cold?
Seasonal allergic rhinitis features clear, watery discharge with intense itching and sneezing “fits”; symptoms begin upon allergen exposure and persist while exposed. Cold (viral rhinitis) has thick, discolored discharge, systemic malaise, and is self-limited to 7–14 days. Allergies recur each season with pollen exposure. - How do tree pollens travel into homes and offices even with windows closed?
Tree pollen grains are microscopic (15–100 micrometers), lightweight, and windborne. They enter through air conditioning systems, ventilation ducts, open doors, and can adhere to clothing and hair, then settle on nasal mucosa indoors. HEPA filters reduce indoor pollen by 85–95%. - Why are tree pollens the “first” allergen season, and when do they peak?
Tree pollens are released earliest in the year as temperatures rise and trees flower. In India, peak tree pollen season is March–April. This precedes grass (May–October) and weed (August–October) seasons, making trees the first seasonal allergen trigger. - What is bagassosis, and how is it different from allergic rhinitis?
Bagassosis is extrinsic allergic alveolitis caused by inhalation of fungal spores and dust particles in sugarcane bagasse. It primarily affects the lungs (alveoli), causing fever, cough, and dyspnea 4–8 hours after exposure. Allergic rhinitis affects nasal/upper airway with sneezing and itching, without fever or systemic illness in simple cases. - How does mast cell degranulation cause symptoms within 5–15 minutes of pollen exposure?
Mast cells have pre-formed granules containing histamine, proteases, and mediators. Upon IgE/allergen cross-linking, granules fuse with the cell membrane and release contents immediately (within minutes). These mediators cause itching, vasodilation (congestion), and mucus secretion rapidly—hence the quick symptom onset. - Can someone become sensitized to tree pollen after just one exposure, or does it require repeated exposure?
Sensitization typically requires repeated or prolonged exposure. First exposure initiates sensitization (IgE production, often silently with no symptoms). Upon subsequent exposures (usually 1–3 weeks later, or in the following pollen season), symptoms develop. However, in highly allergenic environments, some individuals may develop sensitization and symptoms within a single pollen season. - Is it true that antihistamines work better if taken before pollen exposure, rather than after symptoms begin?
Yes. Antihistamines are more effective when prophylactically dosed before allergen exposure. Dosing during early-phase response (first 15 minutes) is less effective because mediator release is rapid and extensive. Pre-season prophylactic use (starting March in tree pollen season) provides better baseline control. Once symptoms develop, antihistamines still help but are not optimally effective for acute severe symptoms. - Why do nasal steroid sprays take 1–2 weeks to work, while antihistamines work within hours?
Antihistamines directly block histamine receptors (immediate effect). Nasal steroids reduce mucosal edema, suppress mast cell mediator production, and reduce inflammatory cell recruitment—all processes requiring several days. Maximum effect at 4 weeks when sustained use allows full anti-inflammatory action. - Can sugarcane workers prevent bagassosis by wearing masks properly, or is the risk still high even with protection?
Proper mask use significantly reduces risk. Research shows workers with proper respiratory protection (N95/FFP2) have 2.31 times lower odds of developing chronic respiratory symptoms compared to unprotected workers. Additionally, workers without proper PPE in areas WITH mechanical ventilation had 3.50 times higher odds than those in ventilated areas—highlighting that engineering controls + PPE together offer best protection. - What is the “allergic salute” and “allergic shiners,” and why do they develop?
Allergic salute: Repeated upward rubbing of the nose with open palm due to nasal itching. Over time, this creates a transverse crease (Dennie’s crease) across the nose bridge. Allergic shiners: Dark circles under eyes due to venous congestion from chronic nasal obstruction. Blood cannot drain efficiently from the lower eyelids, causing discoloration. These signs indicate chronic allergic inflammation. - Why do some tree pollen allergies last for months while others resolve after 2–3 weeks?
Duration depends on pollen season length for that species. Some trees pollinate for 2–3 weeks; others for 6–8 weeks. Additionally, polysensitization (multiple tree pollen sensitivities) extends the season—when one tree’s pollen season ends, another begins, causing continuous symptoms throughout March–May. Monosensitized individuals (one tree pollen) experience shorter symptom duration. - Is immunotherapy (allergy shots or tablets) effective for tree pollen allergies, and how long does treatment take?
Yes. SCIT/SLIT induces significant improvement (60–90%) and long-term tolerance in 60–90% of patients. Treatment duration: 3–5 years of gradual allergen dose escalation. After stopping, clinical benefit persists for years due to immune tolerance. Best candidates: those with multiple seasonal allergen sensitivities or failed maximal medical therapy. - Can someone develop a new allergy to tree pollen later in life, even if they had no symptoms as a child?
Yes. Allergic sensitization can occur at any age. Factors include: cumulative allergen exposure, changes in immune regulation with aging, new environmental exposures (relocating to a high-pollen area), and increased antigen load (climate change increasing pollen production). Some individuals develop symptoms after years of asymptomatic sensitization. - What is the relationship between climate change and tree pollen allergies?
Climate change increases: (1) pollen production (higher CO2 and temperatures enhance pollen yield), (2) earlier pollination start dates (warmer springs trigger earlier flowering), and (3) longer pollen seasons (extended warm periods). These factors increase total atmospheric pollen and extend exposure duration, worsening allergies globally, particularly in temperate/subtropical zones. - Can occupational bagasse exposure cause asthma in previously non-asthmatic workers?
Yes. Occupational exposures (bagasse dust, other organic dusts) can cause occupational asthma through sensitization to dust antigens. Additionally, extrinsic allergic alveolitis (EAA/bagassosis) can lead to reactive airway dysfunction (RADS) with persistent asthma-like symptoms. Prolonged untreated exposure can cause irreversible lung fibrosis, though early recognition and protection prevent progression. - Is it necessary to perform skin prick testing or blood allergy testing to diagnose pollen allergies, or can symptoms alone confirm diagnosis?
Symptoms + temporal relationship to pollen season is often sufficient for diagnosis. However, allergy testing (SPT or serum-specific IgE) is valuable to: (1) confirm sensitization to specific allergens, (2) identify multiple sensitivities (polysensitization), and (3) guide immunotherapy candidates. Testing may be done during or shortly after pollen season (when skin reactivity is highest). - Why do sugarcane workers in India experience more bagassosis than those in developed countries like Australia?
Indian studies report 32–60% of workers develop respiratory symptoms from bagasse exposure [web:190], while Australian studies found no clear chronic bagassosis evidence in sugar workers. Differences likely include: (1) workplace hygiene and ventilation (better in developed countries), (2) PPE availability and compliance, (3) worker safety awareness and training, (4) environmental microbial load (tropical fungal contamination in bagasse), and (5) under-reporting/diagnosis in developing countries. - Can anti-inflammatory medications like NSAIDs reduce allergy symptoms?
NSAIDs provide mild symptom relief (especially for pain/headache accompanying allergies) but do not address the allergic inflammatory cascade. Corticosteroids (nasal sprays) are far more effective. NSAIDs are NOT first-line allergy treatment; antihistamines and nasal steroids are standard. - Why is cromolyn sodium called a “preventive” allergy drug, and when should it be started?
Cromolyn sodium stabilizes mast cells, preventing degranulation. It is most effective prophylactically—started BEFORE anticipated allergen exposure, creating a protective coating on nasal mucosa. Once symptoms and mast cell degranulation have already begun, cromolyn is less effective. Ideal use: start 1–2 weeks before predicted pollen season, not after symptoms develop. - If someone develops symptoms during the sugarcane crushing season and they resolve afterwards, does this confirm occupational bagassosis, or could it be incidental?
Temporal relationship strongly suggests occupational causation. Research confirms symptoms in 60.6% of workers during crushing season vs. 24% post-season, with an odds ratio of 4.79 for bagasse-exposed workers [web:190]. This pattern—symptoms during exposure, resolution during non-exposure—is diagnostic of occupational disease. Confirmation requires spirometry (reduced FEV1) and exclusion of other causes, but temporal pattern is highly suggestive.
FAQ: Hinglish Version (20)
- Seasonal allergic rhinitis (tree pollen से) aur lingering cold में kya difference hai?
Seasonal allergic rhinitis में clear, watery discharge होती है intense itching और sneezing “fits” के साथ; symptoms pollen exposure पर शुरू होते हैं और जब तक exposed न हों तब तक रहते हैं। Cold (viral) में thick, discolored discharge, systemic malaise होता है, और 7-14 दिनों में self-limited। Allergies हर season में pollen exposure से return करते हैं। - Tree pollens घर और offices मेंकैसे enter करते हैं जब windows closed हों?
Tree pollen grains microscopic (15-100 micrometers), lightweight, windborne होते हैं। AC systems, ventilation ducts, open doors से enter करते हैं। Clothing/hair पर adhere होकर indoors settle करते हैं। HEPA filters 85-95% indoor pollen reduce करते हैं। - Tree pollens “first” allergen season क्यों होते हैं, और कब peak होते हैं?
Tree pollens earliest release होते हैं जब temperature rise करता है aur trees flower करते हैं। India में, March-April peak tree pollen season है। यह grass (May-October) और weed (August-October) seasons से पहले आता है। - Bagassosis क्या होता है, aur allergic rhinitis से कैसे अलग है?
Bagassosis extrinsic allergic alveolitis है sugarcane bagasse में fungal spores aur dust inhalation से। Primarily lungs (alveoli) को affect करता है, fever, cough, dyspnea 4-8 hours बाद। Allergic rhinitis nasal/upper airway को sneezing aur itching से, fever या systemic illness नहीं। - Mast cell degranulation कैसे 5-15 minutes में symptoms cause करता है pollen exposure के बाद?
Mast cells mein pre-formed granules होते हैं histamine, proteases से। IgE/allergen cross-linking पर, granules cell membrane से fuse होते हैं aur contents immediately release होता है। ये mediators itching, vasodilation (congestion), mucus secretion rapidly cause करते हैं। - क्या कोई एक exposure से tree pollen को sensitized हो सकता है, या repeated exposure चाहिए?
Sensitization typically repeated या prolonged exposure चाहिए। First exposure sensitization initiate करता है (IgE production, often silently)। Subsequent exposures (usually 1-3 weeks later, या next pollen season), symptoms develop होते हैं। Highly allergenic environments में, कुछ लोग एक pollen season में sensitization aur symptoms develop कर सकते हैं। - क्या antihistamines symptoms के बाद लेने से पहले लेने में ज्यादा effective होते हैं?
Haan। Antihistamines ज्यादा effective होते हैं जब prophylactically allergen exposure से पहले dose किए जाएं। Early-phase response (first 15 minutes) के दौरान dosing कम effective है क्योंकि mediator release rapid aur extensive होता है। Pre-season prophylactic use (March से tree pollen season में) better baseline control provide करता है। - Nasal steroid sprays 1-2 weeks लगता है काम करने में, जबकि antihistamines hours में काम करते हैं क्यों?
Antihistamines directly histamine receptors को block करते हैं (immediate)। Nasal steroids mucosal edema reduce करते हैं, mast cell mediator production suppress करते हैं, inflammatory cell recruitment reduce करते हैं—सभी processes कई दिनों लगते हैं। Max effect 4 weeks में sustained use से। - क्या sugarcane workers masks पहन कर bagassosis prevent कर सकते हैं, या risk फिर भी high है?
Proper mask use से risk significantly reduce होता है। Research दिखाता है workers proper respiratory protection (N95/FFP2) से 2.31 times lower odds chronic respiratory symptoms develop करने का compared to unprotected। PPE + ventilation together best protection offer करते हैं। - “Allergic salute” aur “allergic shiners” क्या होते हैं, aur develop क्यों होते हैं?
Allergic salute: Repeated upward nose rubbing nasal itching से। Over time, transverse crease (Dennie’s crease) bridge पर बन जाता है। Allergic shiners: Dark circles under eyes chronic nasal obstruction से venous congestion से। Blood efficiently drain नहीं कर सकता। - कुछ tree pollen allergies महीनों तक क्यों रहते हैं जबकि कुछ 2-3 हफ्तों में resolve हो जाते हैं?
Duration उस species के pollen season length पर depend करता है। कुछ trees 2-3 हफ्तों के लिए pollinate करते हैं; कुछ 6-8 हफ्ते। Polysensitization (multiple tree sensitivities) season extend करता है—जब एक tree खत्म हो, दूसरा शुरू हो। - क्या Immunotherapy (allergy shots या tablets) tree pollen allergies के लिए effective है, aur कितना time लगता है?
Haan। SCIT/SLIT 60-90% improvement induce करता है। Duration: 3-5 years allergen dose escalation। Stopping के बाद, benefit years तक persist करता है। - क्या कोई later in life नया tree pollen allergy develop कर सकता है, भले ही childhood में कोई symptoms न हों?
Haan। Allergic sensitization कभी भी occur कर सकता है। Factors: cumulative allergen exposure, immune regulation changes, new environmental exposures, increased antigen load (climate change). - Climate change aur tree pollen allergies का relationship क्या है?
Climate change increase करता है: (1) pollen production (higher CO2, temperatures), (2) earlier pollination start dates, (3) longer pollen seasons। ये factors atmospheric pollen total increase करते हैं aur exposure extend करते हैं। - क्या Occupational bagasse exposure non-asthmatic workers में asthma cause कर सकता है?
Haan। Occupational exposures occupational asthma cause कर सकते हैं। Extrinsic allergic alveolitis (EAA/bagassosis) persistent asthma-like symptoms से RADS cause कर सकता है। Prolonged untreated exposure irreversible lung fibrosis cause कर सकता है, though early recognition और protection progression prevent करते हैं। - क्या skin prick testing या blood allergy testing करना necessary है pollen allergies diagnose करने के लिए, या symptoms sufficient हैं?
Symptoms + temporal relationship pollen season से often sufficient है। However, allergy testing (SPT या serum-specific IgE) valuable है: (1) specific allergen sensitization confirm करने के लिए, (2) multiple sensitivities identify करने के लिए, (3) immunotherapy candidates guide करने के लिए। - भारत में sugarcane workers को developed countries जैसे Australia में से ज्यादा bagassosis क्यों है?
Indian studies 32-60% workers respiratory symptoms develop करते हैं , जबकि Australian studies chronic bagassosis नहीं दिखे। Differences: (1) workplace hygiene और ventilation, (2) PPE availability, (3) worker safety awareness, (4) environmental microbial load। - क्या NSAIDs जैसी anti-inflammatory medications allergy symptoms reduce कर सकते हैं?
NSAIDs mild relief provide करते हैं (pain/headache के लिए) लेकिन allergic cascade address नहीं करते। Corticosteroids (nasal sprays) ज्यादा effective हैं। NSAIDs first-line allergy treatment नहीं हैं। - Cromolyn sodium को “preventive” allergy drug क्यों कहा जाता है, aur कब start करना चाहिए?
Cromolyn mast cells को stabilize करता है, degranulation prevent करते हैं। Most effective prophylactically—BEFORE anticipated allergen exposure। Once symptoms शुरू हो गए, cromolyn कम effective है। - Sugarcane crushing season के दौरान symptoms develop हों aur बाद में resolve हों, तो क्या यह bagassosis confirm करता है?
Temporal relationship strongly suggests occupational causation। Research confirms 60.6% workers में crushing season के दौरान symptoms vs. 24% post-season, odds ratio 4.79 bagasse-exposed workers के लिए । यह pattern diagnostic है।
FAQ: हिंदी संस्करण (20)
- Seasonal allergic rhinitis (tree pollen से) और lingering cold में क्या अंतर है?
Seasonal allergic rhinitis में clear, watery discharge होती है intense itching और sneezing “fits” के साथ; लक्षण pollen exposure पर शुरू होते हैं। Cold (viral) में thick, discolored discharge, systemic malaise होता है, और 7-14 दिनों में self-limited। Allergies हर season में pollen exposure से return करते हैं। - Tree pollens घर और offices में कैसे enter करते हैं जब windows closed हों?
Tree pollen grains microscopic (15-100 micrometers), lightweight, windborne होते हैं। AC systems, ventilation ducts से enter करते हैं। Clothing/hair पर adhere होकर indoors settle करते हैं। HEPA filters 85-95% indoor pollen reduce करते हैं। - Tree pollens “first” allergen season क्यों होते हैं, और कब peak होते हैं?
Tree pollens earliest release होते हैं जब temperature rise करता है। भारत में, March-April peak tree pollen season है। यह grass (May-October) seasons से पहले आता है। - Bagassosis क्या होता है, और allergic rhinitis से कैसे अलग है?
Bagassosis extrinsic allergic alveolitis है sugarcane bagasse में fungal spores inhalation से। Primarily lungs (alveoli) को affect करता है, fever, cough, dyspnea 4-8 hours बाद। Allergic rhinitis nasal/upper airway को sneezing और itching से। - Mast cell degranulation कैसे 5-15 minutes में symptoms cause करता है pollen exposure के बाद?
Mast cells में pre-formed granules होते हैं histamine से। IgE/allergen cross-linking पर, granules cell membrane से fuse होते हैं और contents immediately release होता है। ये mediators itching, vasodilation, mucus secretion rapidly cause करते हैं। - क्या कोई एक exposure से tree pollen को sensitized हो सकता है, या repeated exposure चाहिए?
Sensitization typically repeated exposure चाहिए। First exposure sensitization initiate करता है (IgE production, often silently)। Subsequent exposures (usually 1-3 हफ्ते बाद), symptoms develop होते हैं। - क्या antihistamines symptoms के बाद लेने से पहले लेने में ज्यादा effective होते हैं?
हाँ। Antihistamines ज्यादा effective होते हैं जब prophylactically allergen exposure से पहले dose किए जाएं। Early-phase response के दौरान dosing कम effective है क्योंकि mediator release rapid होता है। - Nasal steroid sprays 1-2 हफ्ते लगता है काम करने में, जबकि antihistamines hours में काम करते हैं क्यों?
Antihistamines directly histamine receptors को block करते हैं (immediate)। Nasal steroids mucosal edema reduce करते हैं, inflammatory cells को reduce करते हैं—सभी processes कई दिनों लगते हैं। - क्या sugarcane workers masks पहन कर bagassosis prevent कर सकते हैं?
Proper mask use से risk significantly reduce होता है। Research दिखाता है workers proper respiratory protection से 2.31 times lower odds chronic respiratory symptoms का। - “Allergic salute” और “allergic shiners” क्या होते हैं?
Allergic salute: Repeated upward nose rubbing nasal itching से। Allergic shiners: Dark circles under eyes chronic nasal obstruction से। - कुछ tree pollen allergies महीनों तक क्यों रहते हैं जबकि कुछ 2-3 हफ्तों में resolve हो जाते हैं?
Duration उस species के pollen season length पर depend करता है। Polysensitization season extend करता है। - क्या Immunotherapy (allergy shots) tree pollen allergies के लिए effective है?
हाँ। SCIT/SLIT 60-90% improvement induce करता है। Duration: 3-5 years। - क्या कोई later in life नया tree pollen allergy develop कर सकता है?
हाँ। Allergic sensitization कभी भी occur कर सकता है। Cumulative allergen exposure से। - Climate change और tree pollen allergies का relationship क्या है?
Climate change pollen production, earlier pollination dates, longer seasons increase करता है। - क्या Occupational bagasse exposure non-asthmatic workers में asthma cause कर सकता है?
हाँ। Occupational exposures occupational asthma cause कर सकते हैं। - क्या skin prick testing करना necessary है pollen allergies diagnose करने के लिए?
Symptoms + temporal relationship often sufficient है। Testing specific allergen sensitization confirm करने के लिए valuable है। - भारत में sugarcane workers को developed countries से ज्यादा bagassosis क्यों है?
Workplace hygiene, PPE availability, worker awareness में अंतर है। - क्या NSAIDs allergy symptoms reduce कर सकते हैं?
NSAIDs mild relief provide करते हैं लेकिन allergic cascade address नहीं करते। - Cromolyn sodium “preventive” drug क्यों है?
Cromolyn mast cells को stabilize करता है, degranulation prevent करता है। - Sugarcane season के दौरान symptoms, बाद में resolve—क्या यह bagassosis confirm करता है?
Temporal relationship strongly suggests occupational causation। Research confirms odds ratio 4.79 bagasse-exposed workers के लिए।
PRIME ENT Center Hardoi – Allergy & Occupational Respiratory Care
Address: PRIME ENT Center Hardoi, Hardoi 241001 (Uttar Pradesh), India
For Tree Pollen/Seasonal Allergy Evaluation: Allergy Testing (SPT/Serum IgE), Antihistamine/Steroid Prescription, Immunotherapy Consultation
For Suspected Bagassosis / Occupational Exposure: Spirometry, Chest Imaging (CXR/HRCT), Serum IgG to Thermophilic Actinomycetes, Occupational Health Assessment
For Refractory Allergic Rhinitis: Consider SCIT/SLIT (3–5 year immunotherapy), Endoscopy if structural issues suspected
What to Bring:
- Symptom onset timing relative to pollen season/occupational exposure
- Occupational history (sugarcane mill work, duration, PPE use)
- Previous allergy test results
- List of medications tried
- Environmental/workplace photos if occupational case
Trust PRIME ENT Center Hardoi for Expert Management of Seasonal Pollen Allergies and Occupational Bagassosis
allergic rhinitis tree pollen, bagassosis sugarcane dust, occupational allergy sugarcane, IgE sensitization mast cells, early phase late phase allergy, antihistamine treatment allergic rhinitis, nasal steroid allergy, immunotherapy SCIT SLIT, pollen allergy winter spring India, allergic conjunctivitis eye symptoms, cromolyn sodium allergy, anticholinergic ipratropium, allergic shiners dark circles, allergic salute nasal rubbing, pollen avoidance HEPA filter, dust protective equipment PPE, extrinsic allergic alveolitis EAA, bagasse fibre inhalation, seasonal allergic rhinitis SAR, non-allergic rhinitis NAR, tree pollen calendar India, grass pollen seasons, sensitization IgE antibodies, mast cell degranulation histamine, nasal airway obstruction pollen, nasal itching pruritus sneezing, watery clear rhinorrhea, occupational respiratory disease, respiratory protection mask, sugarcane mill worker health, bagassosis symptoms fever cough