Table of Contents
English Version
Winter Sinus Infections: Why Cold and Dry Air Destroy Your Body’s Natural Defense System and Lead to Sinusitis
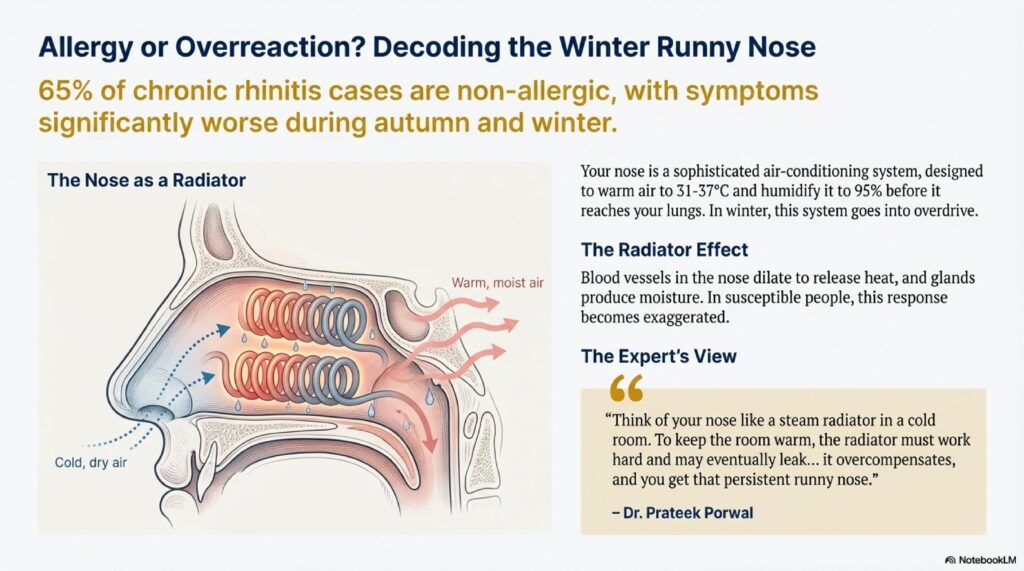
As winter’s harsh grip settles across Hardoi and northern India, ENT clinics experience a predictable surge in sinus-related complaints. Patients arrive describing deep facial pain, thick nasal discharge, and a sensation of pressure in the cheeks and forehead—the classic triad of sinusitis. While many attribute their suffering to a simple “sinus cold” or lingering infection, the clinical reality is far more nuanced: winter sinus infections result from a cascade of physiological failures triggered by cold and dry air, exacerbated by the body’s own impaired defense mechanism—the ciliary system.
At PRIME ENT Center Hardoi, Dr. Prateek Porwal and Dr. Harshita Singh see dozens of patients each winter who ask, “Why does my sinus flare up only in winter?” The answer lies in understanding how the microscopic “sweepers” of the nasal lining—cilia—respond to environmental stress, and how the protective mucous blanket becomes compromised by temperature and humidity extremes.
Part 1: The Architecture of Nasal Defense—Cilia and the Mucous Blanket
Ciliated Epithelium: The First Line of Defense
The entire nasal cavity and paranasal sinuses are lined with a specialized tissue called pseudostratified ciliated columnar epithelium. This single layer of cells performs a critical function: clearing unwanted particles, viruses, and bacteria from the respiratory tract before they reach the lungs.
Every square millimeter of nasal lining contains thousands of ciliated epithelial cells. Each cell is crowned with 50–200 cilia—microscopic, hair-like structures projecting from the cell surface. These cilia are not static; they perform a coordinated, rhythmic “rowing-like” motion, beating at a frequency of 10–20 beats per second (Hz) under normal conditions.
The Mucous Blanket: Two-Layer Architecture
Resting atop the cilia is a protective barrier called the mucous blanket, which consists of two distinct layers:
- The Sol Layer (Deep/Serous Layer): A thin, watery, low-viscosity fluid produced by microvilli. This layer provides the aqueous environment necessary for cilia to beat freely. It comprises approximately 20% of total mucus depth.
- The Gel Layer (Superficial/Viscous Layer): A thicker, more viscous, gelatinous mucus produced by goblet cells and submucosal mucous glands. This layer traps inhaled pollutants, dust particles, bacteria, and viruses. It comprises approximately 80% of mucus depth.
The System in Action: Mucociliary Clearance
The ciliary-mucus system works as a coordinated unit called mucociliary clearance (MCC):
- Directional Beating: Cilia beat in a specific metachronal (wave-like) pattern, pushing the gel layer (and everything trapped within it) in one direction: toward the ostia (natural drainage openings of the sinuses).
- Transport Rate: Under optimal conditions, this system moves mucus at approximately 500 micrometers per second, clearing the entire nasal cavity and sinuses approximately every 30 minutes.
- Final Destination: Mucus eventually reaches the nasopharynx (back of the throat), where it is swallowed and destroyed by stomach acid—a silent, continuous process that goes unnoticed in health.
Why This System Matters
Without effective mucociliary clearance:
- Trapped pathogens multiply
- Inflammatory responses escalate
- Sinus ostia become blocked
- Bacterial superinfection occurs
- Sinusitis develops
Part 2: Winter’s Assault on the Ciliary System
Winter creates a perfect storm for sinus failure. Two environmental changes occur simultaneously: temperature drop and humidity reduction. Both directly sabotage mucociliary clearance.
A. The Effect of Cold Air on Ciliary Beat Frequency
Temperature Sensitivity of Cilia
Cilia are exquisitely temperature-sensitive. Research demonstrates that ciliary beat frequency (CBF) is directly proportional to temperature, with a sigmoidal (S-shaped) relationship:
- At 37°C (normal body temperature): CBF = 8.0–8.1 Hz
- At 32°C (cooled by ~5°C): CBF = 7.6 Hz (≈5% reduction)
- At 25°C (room temperature): CBF = 7.0–7.2 Hz (≈10% reduction)
- At 15°C (very cold): CBF drops to 12.6 Hz (reduction of ~30%)
- Below 10°C: Ciliary movement may cease entirely
Clinical Significance
Even a 5°C drop in nasal mucosal temperature (from inhaling winter cold air) reduces ciliary beat frequency by 5–10%. This seemingly minor change has major consequences:
- Mucus clearance time doubles: Instead of clearing every 30 minutes, mucus may sit in sinuses for 60+ minutes
- Stagnation risk: Prolonged mucus residence time allows trapped viruses and bacteria to multiply
- Secondary bacterial infection: This creates the conditions for acute bacterial rhinosinusitis (ABRS)
The Paradox: Enhanced Mucus Production
Counterintuitively, while cold air slows ciliary beat frequency, the body responds by increasing mucus production to warm the cold air before it reaches the lungs. This creates a “worst of both worlds” scenario:
- Volume: Increased mucus production
- Clearance: Impaired ciliary function
The mismatch overwhelms the system.
B. The Effect of Dry Air on Mucus Viscosity and Ciliary Function
Winter Humidity Crisis
Winter air is extraordinarily dry:
- Outdoor humidity: 15–25% relative humidity in many regions [web:113][web:220]
- Indoor humidity (heated homes/offices): Often drops below 10% [web:113][web:218]
- Optimal humidity for ciliary function: 30–50% relative humidity [web:216][web:218]
This represents a dramatic deficit—the air can hold only 15–25% of the moisture needed for optimal nasal function.
Inspissation: The Thickening of Mucus
In dry conditions, the sol layer (watery component) of the mucous blanket evaporates. When the watery foundation disappears, the overlying gel layer (viscous mucus) becomes extremely thick, tenacious, and “sticky”—a process called inspissation (thickening by evaporation).
Inspissated mucus has these characteristics:
- Viscosity: 10–100 times thicker than normal [web:217]
- Elasticity: Becomes “peanut-butter-like” in consistency
- Stickiness: Adheres to ciliary tips and epithelial surface
Ciliary Entrapment and Dysfunction
When mucus becomes excessively thick from inspissation:
- Cilia become trapped in the sticky secretions, like flies in honey [web:217]
- Metachronal wave pattern is disrupted — the coordinated beating collapses
- Effective clearance stops — cilia beat but accomplish no net mucus transport
Research on cystic fibrosis (a disease characterized by inspissated secretions) demonstrates that even modest mucus hyperconcentration (4–5% solids) compresses the periciliary liquid layer enough to slow mucociliary transport significantly [web:217].
Ciliated Cell Death
Prolonged exposure to dry, cold air can trigger programmed cell death (apoptosis) of ciliated epithelial cells [web:211]. This represents a permanent reduction in the number of “sweepers” available to clear mucus—a deficit that takes weeks to recover once humidity is restored.
Part 3: The Pathological Chain Reaction—From Stasis to Sinus Infection
When the ciliary system fails, a predictable sequence of pathological events unfolds, culminating in acute bacterial rhinosinusitis (ABRS).
Stage 1: Ostial Obstruction and Negative Pressure
- Mucosal Swelling: A viral upper respiratory infection (common cold) causes swelling of the nasal mucosa, particularly around the ostiomeatal complex (OMC)—the final common pathway through which all paranasal sinuses drain.
- Ostia Closure: Combined with environmental cold/dry air effects, the ostia (drainage openings) become progressively obstructed by edematous tissue.
- Negative Pressure Development: Once ostia are sealed, air inside the sinus cavities is slowly absorbed by the sinus lining. Without new air entering through the blocked ostia, negative pressure (vacuum) develops inside the sinus.
- “Vacuum Headache”: This negative pressure manifests clinically as a characteristic deep, throbbing “sinus pressure” or “sinus headache”—often worse when bending forward (gravity increases negative pressure sensation).
Stage 2: Hypo-oxygenation (Low Oxygen)
The oxygen-poor environment inside the blocked sinus becomes progressively more anaerobic (oxygen-depleted). This hypoxic state:
- Impairs mucosal immune function
- Shifts bacteria toward anaerobic metabolism
- Favors growth of oxygen-tolerant pathogens
Stage 3: The Perfect Culture Medium
Within the stagnant, thick, oxygen-poor sinus cavity, conditions are now ideal for bacterial proliferation:
- Nutrient supply: Abundant mucus containing proteins, lipids, minerals
- pH neutrality: Sinus mucus is near-neutral pH
- Temperature: Constant 37°C
- Osmolarity: Isotonic to hypotonic (favorable for bacterial growth)
Stage 4: Bacterial Superinfection
Bacteria that normally inhabit the nasopharynx harmlessly now multiply uncontrollably:
- Streptococcus pneumoniae (30–50% of ABRS cases)
- Haemophilus influenzae (non-typeable strains, 20–30%)
- Moraxella catarrhalis (10–15%)
These bacteria transform the sterile mucus into purulent (pus-filled) discharge—thick, discolored, and often foul-smelling.
Stage 5: Inflammatory Cascade and Symptoms
Bacterial byproducts and inflammatory mediators trigger:
- Mucosal edema (more swelling, worsening obstruction)
- Increased mucus production (inflammatory response)
- Pain signaling from trigeminal nerve endings (facial/head pain)
- Fever (if systemic inflammatory response is severe)
Part 4: Recognizing Winter Sinus Infection—Diagnostic Clues
Cardinal Symptoms of Acute Bacterial Rhinosinusitis (ABRS)
Three major symptoms define ABRS:
- Purulent Nasal Discharge:
- Thick (not watery)
- Discolored (yellow, green, or blood-tinged)
- Visible in nasal cavity or draining into throat (post-nasal drip)
- Facial Pain or Pressure:
- Typically dull, throbbing, and continuous
- Over cheeks (maxillary sinus distribution) or forehead (frontal sinus)
- Worsens when bending forward (gravity increases sinus pressure)
- Often unilateral (one-sided)
- Nasal Obstruction:
- Persistent “naak band” that doesn’t improve with simple nose-blowing
- Often bilateral due to inflammatory edema
- Worse in morning (gravity and stasis overnight)
Minor Associated Symptoms:
- Headache (often severe, throbbing)
- Fever (usually low-grade 38–38.5°C, but can reach 39–40°C)
- Fatigue/malaise
- Dental pain (upper teeth, from maxillary sinus inflammation)
- Cough (from post-nasal drainage, especially at night)
Key Diagnostic Clue: “Double Sickening”
A crucial diagnostic feature is “double sickening” (also called “double worsening”):
- Patient initially has a cold (viral URTI) with typical symptoms (runny nose, cough)
- Days 3–5: Symptoms improve—patient feels better, fever drops
- Days 5–7: Symptoms suddenly worsen with new fever, severe facial pain, thicker purulent discharge
- This pattern strongly suggests bacterial superinfection (ABRS)
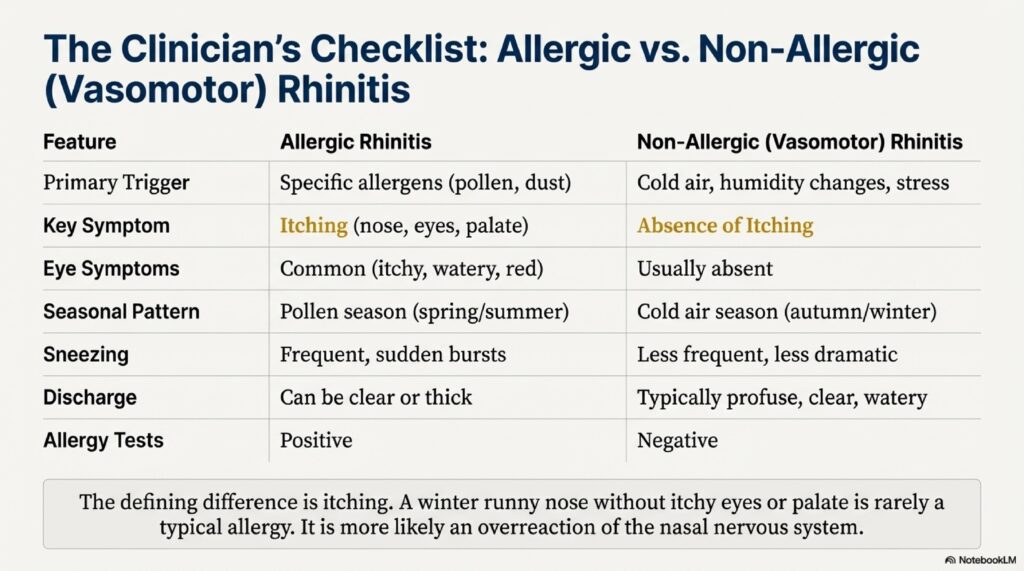
Differentiating from Simple Cold:
| Feature | Viral Rhinitis (Cold) | ABRS (Bacterial Sinusitis) |
|---|---|---|
| Discharge | Clear/watery, then slightly yellow | Thick, purulent (yellow/green) |
| Duration | 7–14 days total | >10 days, worsening |
| Facial pain | Minimal | Severe, localized |
| Fever pattern | Early (days 1–3), resolves | Persists or worsens (days 5+) |
| Worsening pattern | Gradual improvement | “Double sickening” pattern |
| Response to decongestants | Often responsive | Minimal response |
Part 5: Protective Strategies—Restoring the Ciliary System
The goal of winter sinus prevention is to maintain optimal humidity and temperature for ciliary function, and to avoid clogging the already-compromised clearance system.
A. Humidification: Restoring the Sol Layer
Optimal Humidity Range:
- Target: 30–50% relative humidity [web:216][web:218]
- Below 30%: Ciliary dysfunction, mucosal drying
- Above 50%: Risk of mold growth, dust mite proliferation
How to Humidify:
- Home Humidifier:
- Use a cool-mist or warm-mist humidifier in bedroom and main living areas
- Run overnight (8+ hours) when humidity deficit is greatest
- Clean humidifier regularly (weekly) to prevent bacterial/fungal contamination
- Hygrometer (humidity meter): Monitor actual humidity; adjust humidifier accordingly
- Natural Humidity:
- Boiling water on stovetop (during cooking)
- Hot showers/baths (20 minutes daily)
- Drying clothes indoors
- Plants (transpiration adds moisture)
- Avoid Excessive Drying:
- Minimize use of air conditioning (removes humidity)
- Keep bathroom/kitchen exhaust fans on only during necessary times
- Avoid prolonged heating in cars (car heating is extremely drying)
B. Nasal Saline Irrigation—The Cornerstone of Winter Sinus Care
Mechanism:
Saline irrigation physically removes:
- Thick, inspissated mucus
- Viral particles and bacteria
- Inflammatory mediators
- Allergens and irritants
Solution Preparation:
- Warm (not hot) water: 180 mL (1 cup)
- Sodium chloride (salt): 1 teaspoon (≈0.9% isotonic solution)
- Sodium bicarbonate (baking soda): ½ teaspoon (loosens thick mucus, alkalinizes)
- Optional: Sodium biborate (borax): pinch (antiseptic properties)
Technique:
- Use Neti pot, saline rinse bottle (NeilMed), or syringe
- Tilt head forward over sink at 45° angle
- Insert nozzle gently into one nostril
- Allow solution to flow through nasal cavity and out opposite nostril
- Repeat on other side
- Gently blow nose (don’t force) to clear excess solution
Frequency:
- Preventive: 1 time daily (morning or evening)
- During cold/sinus symptoms: 2–3 times daily
- Post-ABRS: Continue 2 weeks after symptoms resolve
Benefits:
- Restores moisture to sol layer
- Promotes ciliary recovery
- Reduces symptom severity by 20–30%
- No systemic side effects
- Inexpensive (~50 rupees per session)
C. Steam Inhalation: Liquefying Inspissated Mucus
Mechanism:
Warm, moist air with aromatic compounds helps to:
- Liquefy thick, sticky mucus
- Increase ciliary beat frequency (warmth effect)
- Reduce mucosal inflammation
- Provide temporary relief
Technique:
- Heat water to steaming (not boiling—too hot damages mucosa)
- Add to water: 2–3 drops Tincture Benzoin, Menthol oil, or Eucalyptus oil
- Technique 1—Bowl Method:
- Pour water into large bowl
- Cover head with towel (tent)
- Breathe steam for 10–15 minutes
- Technique 2—Shower Method:
- Hot shower (let steam fill bathroom)
- Breathe deeply for 10–15 minutes
- Frequency: 2–3 times daily, especially before saline irrigation
Important: Steam provides temporary relief only—it doesn’t replace saline irrigation or humidification for long-term benefit.
D. Hydration: Systemic Fluid Support
Mechanism:
Adequate systemic hydration ensures the body has sufficient water to:
- Produce the watery sol layer
- Maintain mucosal moisture
- Thin secretions for easier clearance
Recommendation:
- Drink 2–3 liters of fluid daily (water, warm tea, broth)
- Avoid caffeine and alcohol (dehydrating)
- Avoid smoking and secondhand smoke (damages ciliated epithelium)
Part 6: What NOT to Do—Avoiding Medicinal Traps
Decongestant Overuse: The Rhinitis Medicamentosa Trap
While topical decongestants (xylometazoline, oxymetazoline) provide rapid symptom relief, they carry a critical warning:
Use Duration: Maximum 3–5 days only [web:213]
What Happens with Prolonged Use:
- Days 1–3: Decongestants work—blood vessels constrict, congestion relieves
- Days 4–5: Body adapts—receptors become less responsive to the medication
- Days 7+: Rebound congestion—upon stopping, blood vessels dilate excessively
- Vicious cycle: User must re-apply spray to relieve rebound congestion
- Rhinitis medicamentosa: Chronic dependence develops; mucosa becomes permanently swollen and dysfunctional
Alternative: Use nasal steroids (fluticasone, mometasone) instead, which work over days and are safe for prolonged use.
Part 7: The “Conveyor Belt” Analogy—Understanding Winter Sinus Dysfunction
To help patients visualize winter sinus problems, Dr. Harshita Singh uses this industrial analogy:
“Imagine your sinus lining as a factory conveyor belt designed to move packages (mucus) out of the building and prevent a pile-up.
In summer: The belt is well-oiled (adequate sol layer), the packages are light and move easily (normal mucus viscosity). The factory hums along smoothly.
In winter: The cold air freezes the motor—the conveyor belt slows dramatically (reduced ciliary beat frequency from cold). At the same time, the dry air turns the packages into heavy, sticky blocks (inspissated mucus). The belt struggles to move these blocks; it gets stuck.
The disaster: Packages pile up on the belt. The belt stops completely. Bacteria begin to colonize the pile of stationary packages—the factory becomes infested (bacterial superinfection).
What happens next: Pressure builds from the pile-up (negative pressure headache). The entire system becomes dysfunctional (ABRS develops).
Treatment restores the system:
- Humidification = “oils the belt” (restores sol layer, improves ciliary function)
- Saline irrigation = “removes the pile” (clears thick mucus, reduces bacterial load)
- Avoiding decongestants = “prevents jamming the mechanism” (avoids making swelling worse)
- Keeping warm indoors = “keeps the motor running” (maintains ciliary beat frequency)
By maintaining humidity, avoiding cold blasts, and regularly clearing the system with saline irrigation, you keep the conveyor belt running smoothly all winter long.”
Hinglish Version
Sardi me Sinus Infection Kyun Badhta Hai: Cold, Dry Air, Aur Ciliary Dysfunction
Winter आता है aur PRIME ENT clinics में sinus-related complaints का surge देखा जाता है। Patients आते हैं deep facial pain, thick nasal discharge, cheeks/forehead में pressure sensation के साथ—sinusitis की classic triad।
Kabhi-kabhi log सोचते हैं कि “simple sinus cold” है, लेकिन clinical reality बहुत अलग है: Winter sinus infections cold aur dry air से trigger होते हैं, जो body के microscopic “sweepers” को fail करते हैं—cilia।
PRIME ENT Center Hardoi में, Dr. Prateek Porwal aur Dr. Harshita Singh dozens of patients देखते हैं जो पूछते हैं: “Mera sinus sirf sardi me kyu flare hota hai?”
Part 1: Nasal Defense—Cilia aur Mucous Blanket
Ciliated Epithelium:
Entire nasal cavity aur sinuses pseudostratified ciliated columnar epithelium से lined होते हैं। Har square millimeter में thousands of ciliated cells होते हैं। Har cell पर 50-200 cilia होते हैं—microscopic hair-like structures जो “rowing-like” motion करते हैं 10-20 beats per second (Hz) पर [web:206][web:208][web:209]।
Mucous Blanket: Two Layers
Cilia के ऊपर mucous blanket होता है जिसके दो layers हैं:
- Sol Layer (Deep/Serous): Thin, watery, low-viscosity fluid। Cilia को freely beat करने का environment।
- Gel Layer (Superficial/Viscous): Thicker, gelatinous mucus। Pollutants, dust, bacteria, viruses को trap करता है।
Mucociliary Clearance (MCC):
Cilia-mucus system coordinated unit है:
- Cilia directional beating से gel layer को ostia (drainage openings) की ओर push करते हैं
- Transport rate: ~500 micrometers/second
- Mucus every 30 minutes clear होता है
- Finally nasopharynx में जाता है, फिर swallow होकर stomach acid में destroy हो जाता है
Part 2: Winter का Assault—Cold aur Dry Air
A. Cold Air का Effect on Ciliary Beat Frequency
Temperature Sensitivity:
Research दिखाता है कि ciliary beat frequency directly proportional होता है temperature को:
- 37°C (normal): CBF = 8.0-8.1 Hz [web:206][web:208]
- 32°C (cooled by ~5°C): CBF = 7.6 Hz (~5% reduction) [web:206]
- 25°C (room temp): CBF = 7.0-7.2 Hz (~10% reduction) [web:206][web:208]
- 15°C (very cold): CBF drops to 12.6 Hz (~30% reduction) [web:208]
- Below 10°C: Ciliary movement completely stop [web:212]
Consequence: Even 5°C drop से ciliary beat frequency 5-10% reduce हो जाता है। Mucus clearance time double हो जाता है—30 minutes से 60+ minutes।
Paradox: Cold air से ciliary function slow होता है, लेकिन body ज्यादा mucus produce करता है (cold air को warm करने के लिए)। Isse volume तो badh जाता है, clearance नहीं—system overwhelmed हो जाता है।
B. Dry Air का Effect—Inspissation
Winter Humidity Crisis:
- Outdoor humidity: 15-25% [web:113][web:220]
- Indoor (heated homes): Often <10% [web:113][web:218]
- Optimal: 30-50% [web:216][web:218]
Inspissation (Thickening):
Dry conditions में sol layer evaporate हो जाता है। Overlying gel layer बहुत thick, sticky, “peanut-butter-like” हो जाता है।
Consequences:
- Viscosity 10-100x thicker normal से [web:217]
- Cilia sticky secretions में trap हो जाते हैं—flies in honey जैसे [web:217]
- Metachronal wave pattern collapse हो जाता है
- Ciliary entrapment: Effective clearance stop हो जाती है
Research दिखाता है कि even modest mucus hyperconcentration (4-5% solids) से mucociliary transport significantly slow हो जाता है [web:217]।
Ciliated Cell Death:
Prolonged dry, cold air से ciliated epithelial cells का apoptosis हो सकता है—permanent reduction ciliary sweepers का।
Part 3: Chain Reaction—From Stasis to Sinus Infection
Stage 1: Ostial Obstruction
- Viral cold से nasal mucosa swell हो जाता है
- Ostiomeatal complex (OMC)—sinus drainage pathway—affected होता है
- Ostia (drainage openings) obstruct हो जाते हैं edema से
Stage 2: Negative Pressure
- Ostia sealed होने से sinus से air absorb हो जाती है
- Negative pressure (vacuum) develop होता है
- “Vacuum headache” = deep, throbbing sinus pressure (बending forward पर worse)
Stage 3: Perfect Culture Medium
Stagnant, thick, oxygen-poor sinus cavity अब ideal bacterial growth environment है।
Stage 4: Bacterial Superinfection
Nasopharyngeal bacteria multiply करना शुरू करते हैं:
- Streptococcus pneumoniae (30-50%)
- Haemophilus influenzae (20-30%)
- Moraxella catarrhalis (10-15%)
Sterile mucus purulent (pus) हो जाता है—thick, yellow/green, foul-smelling।
Stage 5: Inflammation aur Symptoms
- Mucosal edema (more swelling)
- Increased mucus (inflammatory response)
- Facial/head pain (trigeminal nerve)
- Fever (systemic inflammation)
Part 4: Recognizing Winter Sinus Infection
Three Cardinal Symptoms:
- Purulent Nasal Discharge:
- Thick (not watery)
- Discolored (yellow/green/blood-tinged)
- Facial Pain/Pressure:
- Dull, throbbing, continuous
- Over cheeks या forehead
- Worsens bending forward
- Nasal Obstruction:
- Persistent “naak band”
- Doesn’t improve with nose-blowing
- Bilateral (swelling)
Associated Symptoms:
- Headache (severe, throbbing)
- Fever (38-40°C)
- Fatigue
- Dental pain (upper teeth, maxillary sinus से)
- Cough (especially night, post-nasal से)
“Double Sickening” = Key Clue:
- Days 1-3: Viral URTI symptoms start
- Days 3-5: Better होने लगता है
- Days 5-7: Achanak worse होता है new fever, severe facial pain, thick purulent discharge
- Pattern → ABRS (bacterial superinfection)
Part 5: Protective Strategies
A. Humidification
- Target: 30-50% relative humidity [web:216][web:218]
- Cool-mist या warm-mist humidifier bedroom/living areas में
- Hygrometer से monitor करो
- Regularly clean करो (prevent bacterial/fungal contamination)
B. Nasal Saline Irrigation—Cornerstone
Solution:
- 180 mL (1 cup) warm water
- 1 teaspoon salt (0.9% isotonic)
- ½ teaspoon baking soda (loosens mucus)
Frequency:
- Preventive: 1x daily
- During cold: 2-3x daily
- Post-ABRS: 2 weeks continue करो
Benefits:
- Restores sol layer moisture
- Removes thick mucus
- 20-30% symptom reduction
- No side effects
- Cheap
C. Steam Inhalation
- Hot water + Menthol/Eucalyptus/Benzoin
- 10-15 minutes, 2-3x daily
- Liquefies thick mucus
- Temporary relief (not long-term solution)
D. Hydration
- 2-3 liters fluid daily (water, warm tea, broth)
- Avoid caffeine, alcohol (dehydrating)
- Avoid smoking
Part 6: क्या NOT करना चाहिए
Decongestant Overuse:
Maximum 3-5 days only [web:213]
Days 7+ पर rebound congestion होता है—rhinitis medicamentosa (chronic dependence)।
Better: Nasal steroids (fluticasone, mometasone) use करो—safe for prolonged।
Part 7: “Conveyor Belt” Analogy
Sinus lining को factory conveyor belt समझो जो mucus (packages) को बाहर move करता है।
Summer: Belt well-oiled (sol layer), packages light (normal mucus)। Factory smooth चलता है।
Winter: Cold air motor freeze करता है (ciliary slow)। Dry air packages को heavy, sticky blocks बना देता है (inspissated)। Belt stuck हो जाता है।
Disaster: Packages pile-up। Belt stop। Bacteria colonize (सिन्सिटिस)। Pressure build-up (headache)।
Treatment:
- Humidification = “oil the belt” (sol layer restore, cilia improve)
- Saline irrigation = “clear the pile” (thick mucus remove, bacteria clear)
- No decongestants = “prevent jamming” (swelling worse न करो)
- Keep warm = “motor running” (ciliary beat maintain)
हिंदी संस्करण
सर्दी में Sinus Infection क्यों बढ़ता है: Cold, Dry Air, और Ciliary Dysfunction
सर्दी आती है और PRIME ENT clinics में sinus-related complaints का surge देखा जाता है। रोगी आते हैं deep facial pain, thick nasal discharge, गालों/माथे में pressure sensation के साथ—sinusitis की classic triad।
कभी-कभी लोग सोचते हैं कि “simple sinus cold” है, लेकिन clinical reality बहुत अलग है: Winter sinus infections cold और dry air से trigger होते हैं, जो शरीर के microscopic “sweepers” को fail करते हैं—cilia।
PRIME ENT Center Hardoi में, डॉ प्रतीक पोरवाल और डॉ हर्षिता सिंह dozens of patients देखते हैं जो पूछते हैं: “Mera sinus sirf sardi me kyu flare hota hai?”
Part 1: Nasal Defense—Cilia और Mucous Blanket
Ciliated Epithelium:
पूरी nasal cavity और sinuses pseudostratified ciliated columnar epithelium से lined होते हैं। हर square millimeter में thousands of ciliated cells होते हैं। हर cell पर 50-200 cilia होते हैं—microscopic hair-like structures जो “rowing-like” motion करते हैं 10-20 beats per second (Hz) पर [web:206][web:208][web:209]।
Mucous Blanket: Two Layers
Cilia के ऊपर mucous blanket होता है जिसके दो layers हैं:
- Sol Layer (Deep/Serous): Thin, watery, low-viscosity fluid। Cilia को freely beat करने का environment।
- Gel Layer (Superficial/Viscous): Thicker, gelatinous mucus। Pollutants, dust, bacteria, viruses को trap करता है।
Mucociliary Clearance (MCC):
Cilia-mucus system coordinated unit है:
- Cilia directional beating से gel layer को ostia (drainage openings) की ओर push करते हैं
- Transport rate: ~500 micrometers/second
- Mucus every 30 minutes clear होता है
- Finally nasopharynx में जाता है, फिर swallow होकर stomach acid में destroy हो जाता है
Part 2: Winter का Assault—Cold और Dry Air
A. Cold Air का Effect on Ciliary Beat Frequency
Temperature Sensitivity:
Research दिखाता है कि ciliary beat frequency directly proportional होता है temperature को:
- 37°C (normal): CBF = 8.0-8.1 Hz [web:206][web:208]
- 32°C (cooled by ~5°C): CBF = 7.6 Hz (~5% reduction) [web:206]
- 25°C (room temp): CBF = 7.0-7.2 Hz (~10% reduction) [web:206][web:208]
- 15°C (very cold): CBF drops to 12.6 Hz (~30% reduction) [web:208]
- Below 10°C: Ciliary movement पूरी तरह stop [web:212]
Consequence: Even 5°C drop से ciliary beat frequency 5-10% reduce हो जाता है। Mucus clearance time double हो जाता है—30 minutes से 60+ minutes।
Paradox: Cold air से ciliary function slow होता है, लेकिन body ज्यादा mucus produce करता है (cold air को warm करने के लिए)। इससे volume तो बढ़ जाता है, clearance नहीं—system overwhelmed हो जाता है।
B. Dry Air का Effect—Inspissation
Winter Humidity Crisis:
- Outdoor humidity: 15-25% [web:113][web:220]
- Indoor (heated homes): Often <10% [web:113][web:218]
- Optimal: 30-50% [web:216][web:218]
Inspissation (Thickening):
Dry conditions में sol layer evaporate हो जाता है। Overlying gel layer बहुत thick, sticky, “peanut-butter-like” हो जाता है।
Consequences:
- Viscosity 10-100x thicker normal से [web:217]
- Cilia sticky secretions में trap हो जाते हैं—flies in honey जैसे [web:217]
- Metachronal wave pattern collapse हो जाता है
- Ciliary entrapment: Effective clearance stop हो जाती है
Research दिखाता है कि even modest mucus hyperconcentration (4-5% solids) से mucociliary transport significantly slow हो जाता है [web:217]।
Ciliated Cell Death:
Prolonged dry, cold air से ciliated epithelial cells का apoptosis हो सकता है—permanent reduction ciliary sweepers का।
Part 3: Chain Reaction—From Stasis to Sinus Infection
Stage 1: Ostial Obstruction
- Viral cold से nasal mucosa swell हो जाता है
- Ostiomeatal complex (OMC)—sinus drainage pathway—affected होता है
- Ostia (drainage openings) obstruct हो जाते हैं edema से
Stage 2: Negative Pressure
- Ostia sealed होने से sinus से air absorb हो जाती है
- Negative pressure (vacuum) develop होता है
- “Vacuum headache” = deep, throbbing sinus pressure (झुकने पर worse)
Stage 3: Perfect Culture Medium
Stagnant, thick, oxygen-poor sinus cavity अब ideal bacterial growth environment है।
Stage 4: Bacterial Superinfection
Nasopharyngeal bacteria multiply करना शुरू करते हैं:
- Streptococcus pneumoniae (30-50%)
- Haemophilus influenzae (20-30%)
- Moraxella catarrhalis (10-15%)
Sterile mucus purulent (pus) हो जाता है—thick, yellow/green, foul-smelling।
Stage 5: Inflammation और Symptoms
- Mucosal edema (more swelling)
- Increased mucus (inflammatory response)
- Facial/head pain (trigeminal nerve)
- Fever (systemic inflammation)
Part 4: Recognizing Winter Sinus Infection
Three Cardinal Symptoms:
- Purulent Nasal Discharge:
- Thick (not watery)
- Discolored (yellow/green/blood-tinged)
- Facial Pain/Pressure:
- Dull, throbbing, continuous
- Over cheeks या forehead
- झुकने पर worse
- Nasal Obstruction:
- Persistent “नाक बंद”
- Nose-blowing से improve नहीं
- Bilateral (swelling)
Associated Symptoms:
- Headache (severe, throbbing)
- Fever (38-40°C)
- Fatigue
- Dental pain (upper teeth, maxillary sinus से)
- Cough (especially night, post-nasal से)
“Double Sickening” = Key Clue:
- Days 1-3: Viral URTI symptoms शुरू
- Days 3-5: बेहतर होने लगता है
- Days 5-7: Achanak worse होता है new fever, severe facial pain, thick purulent discharge
- Pattern → ABRS (bacterial superinfection)
Part 5: Protective Strategies
A. Humidification
- Target: 30-50% relative humidity [web:216][web:218]
- Cool-mist या warm-mist humidifier bedroom/living areas में
- Hygrometer से monitor करो
- Regularly clean करो (prevent bacterial/fungal contamination)
B. Nasal Saline Irrigation—Cornerstone
Solution:
- 180 mL (1 cup) warm water
- 1 teaspoon salt (0.9% isotonic)
- ½ teaspoon baking soda (loosens mucus)
Frequency:
- Preventive: 1x daily
- During cold: 2-3x daily
- Post-ABRS: 2 weeks continue करो
Benefits:
- Restores sol layer moisture
- Removes thick mucus
- 20-30% symptom reduction
- No side effects
- Cheap
C. Steam Inhalation
- Hot water + Menthol/Eucalyptus/Benzoin
- 10-15 minutes, 2-3x daily
- Liquefies thick mucus
- Temporary relief (not long-term solution)
D. Hydration
- 2-3 liters fluid daily (water, warm tea, broth)
- Avoid caffeine, alcohol (dehydrating)
- Avoid smoking
Part 6: क्या NOT करना चाहिए
Decongestant Overuse:
Maximum 3-5 days only [web:213]
Days 7+ पर rebound congestion होता है—rhinitis medicamentosa (chronic dependence)।
Better: Nasal steroids (fluticasone, mometasone) use करो—safe for prolonged।
Part 7: “Conveyor Belt” Analogy
Sinus lining को factory conveyor belt समझो जो mucus (packages) को बाहर move करता है।
Summer: Belt well-oiled (sol layer), packages light (normal mucus)। Factory smooth चलता है।
Winter: Cold air motor freeze करता है (ciliary slow)। Dry air packages को heavy, sticky blocks बना देता है (inspissated)। Belt stuck हो जाता है।
Disaster: Packages pile-up। Belt stop। Bacteria colonize (sinusitis)। Pressure build-up (headache)।
Treatment:
- Humidification = “oil the belt” (sol layer restore, cilia improve)
- Saline irrigation = “clear the pile” (thick mucus remove, bacteria clear)
- No decongestants = “prevent jamming” (swelling worse न करो)
- Keep warm = “motor running” (ciliary beat maintain)
FAQ: English Version (20)
- What is ciliary beat frequency (CBF), and why does it matter for sinus health?
Ciliary beat frequency is the number of times cilia beat per second (measured in Hz). Normal CBF at body temperature (37°C) is 8.0-8.1 Hz. Research shows CBF is highly temperature-dependent: dropping 5% at 32°C and 10% at 25°C [web:206]. Reduced CBF means slower mucus clearance, allowing mucus to stagnate and bacteria to multiply. - How much does ciliary beat frequency decrease in cold air?
For every 5°C drop in mucosal temperature from 37°C, CBF decreases approximately 5-10%. At 25°C (room temperature), CBF is reduced by 10% [web:206]. At 15°C (very cold), reduction can reach 30% [web:208]. Below 10°C, ciliary movement may cease entirely [web:212]. - What is the “sol layer” and “gel layer” of the mucous blanket?
The sol layer is a thin, watery, low-viscosity fluid beneath the cilia that allows them to beat freely. The gel layer is a thicker, more viscous mucus that traps pollutants, bacteria, and viruses. In dry conditions, the sol layer evaporates, causing the overlying gel layer to become thick and inspissated (thickened), trapping cilia. - What does “inspissation” mean, and why is it dangerous for sinus health?
Inspissation is the thickening of mucus through evaporation of its watery components. Inspissated mucus becomes “peanut-butter-like” in consistency—10-100 times thicker than normal [web:217]. Cilia become trapped in this sticky mucus like “flies in honey” and cannot beat effectively, halting mucociliary clearance and allowing bacterial overgrowth. - Why does the nose produce MORE mucus when breathing cold air?
Cold air triggers parasympathetic nerve stimulation, causing increased mucus production. The body responds to cold air by making extra mucus to warm it before it reaches the lungs. However, simultaneously, ciliary beat frequency decreases, creating a mismatch: increased volume + decreased clearance = system overload. - What is the “ostiomeatal complex” (OMC) and why is it important?
The OMC is the final common pathway through which the paranasal sinuses drain into the nasopharynx. When viral cold causes mucosal swelling, the OMC becomes obstructed, blocking sinus drainage. This leads to fluid accumulation, negative pressure, and bacterial superinfection. - What is “negative pressure” in the sinuses, and what symptoms does it cause?
When ostia (sinus drainage openings) are blocked, air inside the sinus is absorbed by the lining, creating a vacuum (negative pressure). This manifests clinically as a characteristic “sinus pressure headache”—often worse when bending forward (gravity increases negative pressure sensation). - How does the “double sickening” pattern help diagnose bacterial sinusitis?
“Double sickening” is a diagnostic clue for acute bacterial rhinosinusitis (ABRS): patient has viral cold for days 1-3, feels better days 3-5, then suddenly worsens days 5-7 with new fever, severe facial pain, and purulent discharge. This pattern indicates bacterial superinfection of stagnant viral fluid. - What bacteria most commonly cause winter sinus infections?
The three most common bacteria in ABRS are Streptococcus pneumoniae (30-50%), Haemophilus influenzae non-typeable strains (20-30%), and Moraxella catarrhalis (10-15%). These bacteria normally inhabit the nasopharynx but multiply excessively when conditions (low oxygen, stagnant thick mucus) favor their growth. - Why is winter humidity often below 30%, and what is the optimal level?
Winter outdoor air naturally holds less moisture (15-25% RH). Indoor heating further dries air by warming it without adding moisture, sometimes dropping humidity below 10%. Research shows mucociliary clearance functions optimally at 30-50% relative humidity [web:216][web:218]. - Does humidification actually improve mucociliary clearance?
Yes. Research demonstrates that humidity levels of at least 30% are needed for adequate mucociliary clearance; 45-50% RH is optimal [web:216]. Humidifiers reduce mucus viscosity and prevent ciliary dysfunction caused by dryness. - What is the proper technique for nasal saline irrigation?
Use warm isotonic (0.9%) or hypertonic (2.3%) saline solution with 1-2 drops baking soda. Tilt head forward 45°, insert nozzle gently, allow solution to flow through cavity and exit opposite nostril. Use once daily preventively, 2-3x during cold/sinusitis. - Is steam inhalation effective for thick winter sinus mucus?
Steam provides temporary relief by warming airways and humidifying air, helping liquefy thick mucus. However, effects are short-lived (minutes to hours). Steam should complement saline irrigation and humidification, not replace them. Benefits are primarily symptomatic relief, not disease treatment. - Why is decongestant overuse dangerous, and what is “rebound congestion”?
Topical decongestants (xylometazoline) should be used maximum 3-5 days. Prolonged use causes the nasal mucosa to adapt (receptor desensitization). Upon stopping, blood vessels dilate excessively (rebound), causing worse congestion than before. This creates “rhinitis medicamentosa”—chronic decongestant dependence. Use nasal steroids instead for prolonged therapy. - Can cold-induced ciliary dysfunction be permanently reversed?
Yes. Ciliary beat frequency recovers to normal once nasal mucosa temperature is restored and humidity is adequate. Research shows that if cilia are kept at appropriate temperature and moisture, CBF can recover over hours to days. However, prolonged very cold/dry exposure can cause ciliated cell death, which requires weeks for epithelial regeneration. - Why do sinusitis symptoms often worsen at night in winter?
Overnight, gravity causes mucus to pool in sinuses while the patient lies flat. Additionally, winter humidity is often lowest at night (heating systems run, outdoor humidity low). Stagnant, thick mucus accumulates undrained, causing pressure and pain that peak upon waking. - Is it normal for nasal discharge to change color from clear to yellow/green during a winter cold?
Color change alone doesn’t distinguish viral from bacterial infection. Viral colds can produce yellowish discharge in later stages (days 3-7) due to inflammatory debris and dead white blood cells, not necessarily bacterial infection. The key is symptom duration and pattern: viral resolves by day 14; bacterial (ABRS) worsens after initial improvement (double sickening). - Can chronic winter sinusitis increase the risk of serious complications?
Yes. Untreated chronic sinusitis can lead to: orbital cellulitis (eye involvement), meningitis (brain infection spread), cavernous sinus thrombosis, and permanent ciliary damage. However, most winter sinusitis resolves with medical management; complications are rare with appropriate care. - Why might someone with recurrent winter sinusitis benefit from year-round humidity maintenance, not just winter?
Some individuals have persistent ciliary dysfunction or structural abnormalities (e.g., deviated septum, narrow ostia). These patients benefit from maintaining near-optimal humidity (40-50%) year-round to maximize residual mucociliary clearance. This may reduce infection frequency by 40-50%. - If home humidification and saline irrigation don’t relieve winter sinusitis, when should imaging or specialist care be sought?
If symptoms persist >10-14 days despite maximal medical therapy (humidification, saline ≥3x daily, nasal steroids, hydration), evaluation should include nasal endoscopy and possibly CT sinus imaging. Red flags include severe unilateral pain, fever >39°C, facial swelling, eye symptoms, or altered mental status (possible complications).
PRIME ENT Center Hardoi – Winter Sinus Care
Address: PRIME ENT Center Hardoi, Hardoi 241001 (Uttar Pradesh), India
For Winter Sinus Symptoms: Humidification Consultation, Saline Irrigation Technique Training, Nasal Endoscopy if Indicated
For Recurrent Winter Sinusitis: CT Sinus Imaging, Nasal Endoscopy Assessment, Possible FESS if Structural Obstruction
For Acute Severe Sinusitis (Red Flags): Same-Day Evaluation, Imaging, Possible IV Antibiotics
What to Bring:
- Symptom timeline (when started, progression pattern)
- Previous sinus imaging/endoscopy results
- List of medications tried (especially decongestants)
- Humidifier/humidity measurement device
- Environmental history (office/home heating systems)
Trust PRIME ENT Center Hardoi for Expert Winter Sinus Management and Ciliary Function Optimization
Secondary Keywords (Comma-Separated):
ciliary beat frequency temperature, mucociliary clearance dry air winter, inspissation thick mucus, sol layer gel layer mucous blanket, pseudostratified ciliated epithelium, cilia microscopic sweepers, nasal sinuses anatomy, ostiomeatal complex OMC drainage, ostia sinus openings, double sickening bacterial infection, acute bacterial rhinosinusitis ABRS, bacterial superinfection virus, Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, negative pressure vacuum sinus headache, stagnant mucus culture medium bacteria, ciliary entrapment sticky mucus, ciliated cell death viral bacterial, humidifier indoor humidity 30-50%, saline nasal irrigation alkaline wash, steam inhalation menthol eucalyptus, nasal decongestant xylometazoline overuse, rhinitis medicamentosa rebound, winter humidity levels 15-25%, sinus ostia obstruction swelling, OMC ostiomeatal complex blockage, hypo-oxygenation anoxia sinus, winter respiratory infections peak, cold air mucus viscosity thickness, ciliary dysfunction winter sinusitis, mucociliary conveyor belt analogy